16 April 2024: Clinical Research
Comparative Analysis of Transoral Endoscopic Parathyroidectomy Vestibular Approach and Focused Open Surgery for Primary Hyperparathyroidism Treatment: A Single Center Experience
Mehmet Zafer SabuncuogluDOI: 10.12659/MSM.944128
Med Sci Monit 2024; 30:e944128
Abstract
BACKGROUND: Primary hyperparathyroidism is one of the most common endocrine disorders, for which the definitive treatment is surgical parathyroidectomy. Generally, surgical exploration is performed as open focused neck surgery. The vestibular route is a new approach to minimally invasive endoscopic parathyroidectomy. This retrospective study from a single center in Turkey aimed to compare surgical outcomes from the transoral endoscopic vestibular approach (TOEPVA) vs direct open parathyroidectomy in 57 patients.
MATERIAL AND METHODS: Our study included data from 57 patients. TOEPVA was performed in 20 of these patients who did not want a cervical scar, and focused surgery was performed in the remaining 37 patients. The variables we analyzed were size, volume, and localization of the adenoma, operative time, presence of bleeding, presence of the recurrent laryngeal nerve damage, preoperative, short-term, and long-term postoperative PTH levels, use of drain, presence of postoperative hypocalcemia, and short-term and long-term calcium levels.
RESULTS: No laryngeal nerve and mental nerve damage was observed in either group. The mean operative time in focused open surgery was 80.54±33.1 min, while the mean operative time in TOEPVA was 128.21±30.88 (p: 0.794) min. The mean hospitalization period of patients who underwent open surgery was 3.29±1.9 days, while the mean discharge days of patients who underwent endoscopic surgery was 2.40±1.2. (p>0.05).
CONCLUSIONS: TOEPVA is a safe method in patients who underwent parthyroid surgery to avoid cervical scarring.
Keywords: endoscopy, Hyperparathyroidism, Parathyroidectomy
Introduction
There are numerous techniques used for parathyroidectomy, including unilateral or bilateral open cervical exploration, gamma probe-guided minimally invasive open surgery, video-assisted minimally invasive surgery, and endoscopic surgery via axillary approach.
With the development of imaging techniques and intraoperative parathyroid hormone monitoring, a minimally invasive approach can be used in parathyroid surgery [1–3], achieving similar effective treatment rates with smaller incisions, shorter operation time, and faster recovery [4,5].
With the increasing use of endoscopic devices, alternative approaches have gained importance to prevent scar formation in thyroid and parathyroid surgery. In the last 20 years, endoscopic methods such as transaxillary, breast-chest, aerola, and sublingual approaches have been described for parathyroid surgery [6]. However, these methods have not been widely used due to the long learning time, long operation time, large dissection area, and uncertainty.
In 2016, Angkoon Anuwong published the first case series of patients who underwent thyroid and parathyroid surgery via the transoral vestibular approach [3,6,7]. After this published case series, ‘visible scarless surgery’ has become increasingly common in different centers with encouraging results. With approximately 900 reported cases, TOEPVA attracts patients who seek to avoid neck scarring [8]. Therefore, this retrospective study from a single center in Turkey aimed to compare surgical outcomes from the transoral endoscopic vestibular approach with direct open parathyroidectomy in 57 patients.
Material and Methods
PREOPERATIVE EVALUATION AND CONSIDERATIONS:
All patients with parathyroid adenoma and parathyroid hyperplasia were informed about the 2 surgical approaches to correct the existing condition. One is a focused cervical surgery with an incision of approximately 2 cm, and the other is TOEPVA. When selecting the TOEPVA method in patients, the eligibility criteria included being over 18 years of age, patient willingness, appropriate neck structure, appropriate jaw structure, patient weight, and the size of the defined lesion. Contraindications were limited to previous neck surgery, history of neck radiation, history of thyroiditis, and patients without consent. There was no limitation for focused open surgery.
We explained that the main difference between the 2 procedures is that an incision is made on the adenoma in the cervical approach, resulting in a cervical scar. In contrast, a larger tissue dissection is performed in the transoral method, and there is no cervical scar. The choice between the 2 procedures was left to patients, who were suitable for both procedures.
Preoperative localization is a critical component of successful minimally invasive parathyroid surgery. By utilizing various imaging techniques and, when necessary, invasive methods, surgeons can accurately identify the affected parathyroid gland(s) and perform a targeted and minimally invasive procedure, leading to improved patient outcomes [9]. Ultrasound and scintigraphy were used in preoperative patient evaluation for all patients in both group. The scintigraphy images of the patients were examined by a single interventional radiologist (DG). Before surgery, marking was done with methylene blue under ultrasonography (Toshiba Xario 200-Japan) by a 22G needle.
SURGICAL TECHNIQUE:
When performing the TOEPVA procedure, the patient was prepared under general anesthesia for orotracheal intubation in a supine position with a slight neck extension. Preoperatively, patients received prophylactic antibiotic therapy with amoxicillin-clavulanic acid [10]. Three incisions were made in the lower lip. To prevent lip burn, the midline incision was created as a 10 mm incision just above the frenulum towards the oral vestibule (Figure 1). The other incisions were made with two 5-mm vertical incisions on the lateral aspect of the canines, almost at the level of the first molar, to prevent mental nerve damage and tearing of the lip commissures [10]. Some authors recommend and even specifically encourage using intraoperative nerve monitoring (IONM) when using the TOEPVA technique [11]. Thus, these access points achieved neck access through 3 incisions. Hydrodissection was performed by administering adrenaline saline solution (100 ml 1: 1000 adrenaline/normal saline) with a veres needle to the dissection areas by accepting the suprasternal notch inferiorly, the anterior edge of the sternocleidomastoid muscle on both lateral sides, and the larynx on the superior side. Trocar placements were made after hydrodissection (Video 1). An 11-mm trocar for the 30-degree camera was placed in the frenulotomy and lateral port sites, and two 5-mm trocars were placed for the working ports. Subsequently, insufflation with 6 mmHg CO2 was performed. The dissection of the relevant area was completed with blunt and sharp dissections (Video 2).
Following neck dissection, insufflation with 6 mmHg CO2 was performed. The fibrous bands between the subplatysmal area were opened with a hook coetry. Two pieces of 0/0 prolene were used as mechanical slings to enlarge the dissection area. The other stages of surgery were similar to a focused open parathyroidectomy. After all preparations, the thyroid lobe of the involved side was dissected and lifted towards the medial side. With the help of ultrasound, the parathyroid tissue was localized and marked with methylene, de-vascularized, and excised (Video 3). Each specimen was removed from the 10-mm trocar entry site with the help of a minibag. After bleeding control, the dissected muscles were closed with a midline 3/0 vloc suture. After controlling bleeding in the lip mucosa, the incisions were closed with 4/0 absorbable suture material (monocryl) (Figure 2). The operation ended with a pressure dressing on the dissection area. In the postoperative period, the need for antibiotic use, importance of wound care, and regular neck exercise were emphasized [12].
Focused surgery was performed on the gland, which was localized preoperatively by scintigraphy and ultrasound and marked with methylene blue by ultrasound. The surgical procedure began with a 2–3 cm incision following Kocher’s technique, typically 2 cm above the sternal notch. For parathyroid adenomas located higher up in the neck or behind the esophagus, the incision was placed along the front edge of the sternocleidomastoid muscle. The strap muscles in the neck were carefully dissected but not severed. The thyroid gland was then mobilized to expose the area of interest. Once visualized, the parathyroid adenoma was identified, dissected free from surrounding tissue, removed, weighed, and sent for a rapid analysis (frozen section) to confirm the diagnosis. The parathyroid glands were not explored.
PATIENTS:
This retrospective study was conducted over 48 months between August 2018 and June 2022 in the tertiary general surgery department of Suleyman Demirel University; 37 patients preferred the cervical approach, and 20 patients preferred the transoral vestibular approach (Figure 3).
Written informed consent was obtained from all patients to perform this surgery and to use their data in this study. All clinical, operative, pathological, and follow-up data were categorized from our populated database.
The routine physical examination findings of the patients were evaluated to check for complications such as recurrent laryngeal nerve damage. Laryngoscopic examination was not performed in patients without symptoms.
STATISTICS:
The data were transferred to IBM SPSS.23 (IBM, Inc., Chicago, IL, USA) and evaluated by statistical analysis. Before statistical analyses, we checked for correct data entry and parameters within the expected range. Normality assumptions of continuous variables were examined by the Shapiro-Wilk test and homogeneity of variance by Levene’s test. Mean, standard deviation (SD), median, and IQR were used in the descriptive statistics of continuous variables, and frequency (n) and percentage (%) values were used in the descriptive statistics of categorical variables. The
Results
DEMOGRAFIC FINDINGS:
We performed 57 parathyroidectomies with 37 focused cervical approaches and 20 transoral vestibular approaches. Ten patients who underwent focused parathyroid surgery were excluded from the study because they did not have screening scintigraphy and did not meet the inclusion criteria. During this study, the TOEPVA procedure was performed by a single operator (Figure 1).
There were 51 female and 6 male patients. TOEPVA was performed in 20 female patients, while the classical cervical approach was preferred by all male patients.
The mean age of patients who underwent open surgery (group 1) was 57.2±12.5 years, while the mean age of patients who underwent endoscopic surgery (group 2) was 49.9±6.8 years, and the difference was not statistically significant.
CLINICAL OUTCOMES:
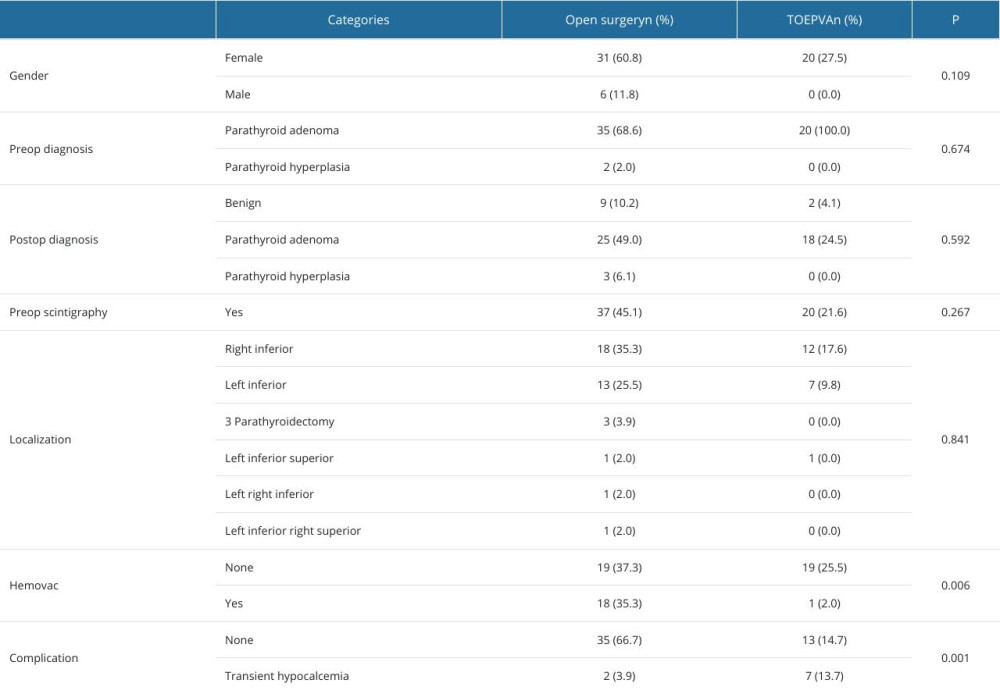
In 55 patients, the preoperative diagnosis was parathyroid adenoma. Parathyroid scintigraphy and ultrasound were available preoperatively. All scintigraphy results were compatible with parathyroid adenoma. Classical surgery was performed in 37 patients and TOEPVA in 20 patients. The postoperative diagnoses of the patients who underwent classical surgery were parathyroid adenoma in 25, benign in 9, and parathyroid hyperplasia in 3. Among patients undergoing TOEPVA, the postoperative diagnosis of 18 patients was compatible with parathyroid adenoma, and the postoperative tissue diagnosis of the other patients was benign (Table 1).
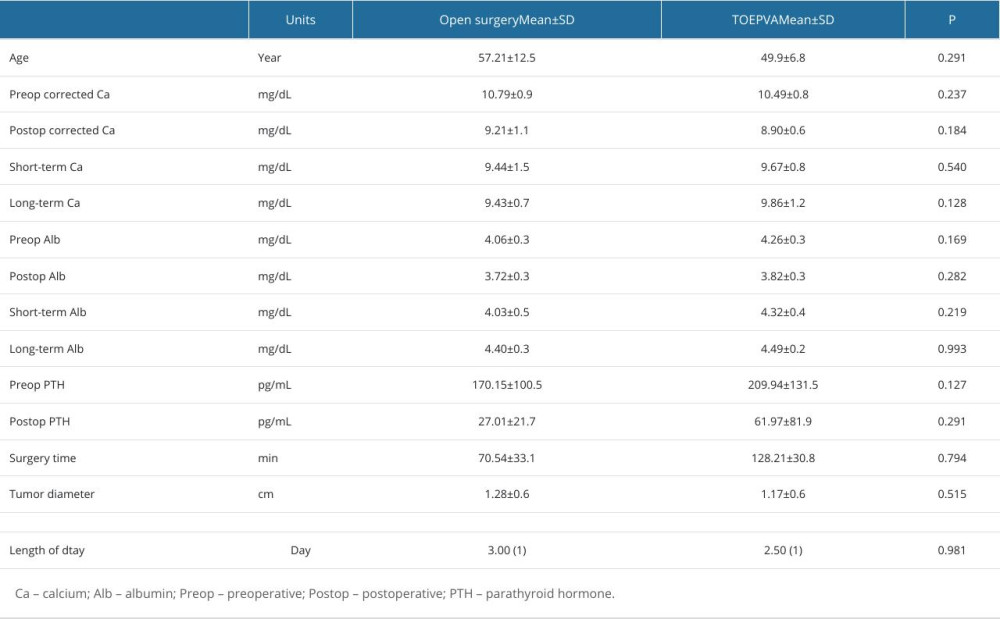
Mean preoperative calcium was 10.8±0.9 mg/dL, postoperative calcium was 9.2±1.1 mg/dL, short-term calcium was 9.4±1.5 mg/dL, and long-term calcium was 9.43±0.7 mg/dL in patients who underwent open surgery. In patients who underwent endoscopic surgery, mean preoperative calciul was 10.5±0.8 mg/dL, postoperative calcium was 8.9±0.6 mg/dL, short-term calcium was 9.7±0.8 mg/dL, and long-term calcium was 9.9±1.2 mg/dL. The choice of surgical method had no significant effect on the results (
In patients who underwent open surgery, mean preoperative PTH was 170.1±100.5 pg/mL and mean postoperative was 27±21.7 pg/mL. In patients who underwent endoscopic surgery, mean preoperative PTH was 209.9±131.5 pg/mL and mean postoperative PTH was 62.0±81.9 pg/mL. There was no significant effect of the surgical method on the results (
Intraoperative PTH could not be measured in both types of operations because it was not available at the institution where the operation was performed, but it was assessed at postoperative follow-up. Postoperative corrected calcium levels were also monitored.
The mean operative time was 80.5±33.1 min in open surgery and 128.2±30.8 min in endoscopic surgery.
In open surgery, lesions identified preoperatively were excised; bilateral neck exploration was not performed. The median hospitalization period of patients who underwent open surgery was 3 days, while the median discharge days of patients who underwent endoscopic surgery was 2.5 days. Neither surgical method was superiorer in terms of length of hospitalization (
All patients who underwent TOEPVAe resumed oral intake on postoperative day 1, while patients who underwent focused surgery resumed oral intake 8 h after surgery.
No complications were observed in 48 patients in the early postoperative period. However, a soft-tissue infection was observed in 1 patient in the late postoperative period. Transient hypocalcemia was observed in 2 patients after classical surgery and 7 patients after TOEPVA. Calcium values were calculated as corrected calcium. Transient hypocalcemia status returned to normal levels within 6 months (Table 2).
Discussion
This study compared the results of focused open parathyroid surgery and TOEPVA and the risks that may occur in patients. In our study, there was no difference between focused open surgery and TOEPVA in terms of complications. Except for the long operation time, the TOEPVA technique is as safe as focused surgery. Our study shows TOEPVA is a safe scarless surgical alternative to open parathyroidectomy.
The field has undergone significant development from traditional open surgery to minimally invasive techniques, driven by passionate surgeons. While open surgery remains prevalent worldwide, various endoscopic and robotic techniques have emerged. Even newer approaches like thoracoscopic, robotic, and specific neck incision points are being explored. Minimally invasive approaches, particularly focused mini-parathyroidectomy and minimally invasive neck parathyroidectomy, are gaining favor due to their benefits. These techniques strive to achieve the best cosmetic outcome (minimal scarring) while ensuring successful treatment and low complication rates. The idea of minimally invasive parathyroidectomy (MIPT) emerged from the desire to reduce incision size and utilize video assistance. While initial studies demonstrated significantly improved cosmetic satisfaction without increased complications, the higher cost due to specialized instruments remains a factor. As the technology for MIPT evolves, the cost may become similat to that of traditional approaches [13].
There are no large study series on TOEPVA, but complication rates in studies for TOEPVA ranged from 5% to 44.6% [7]. The most common complications in these studies were recurrent laryngeal nerve injury, seroma, hematoma, CO2 embolism, subcutaneous emphysema, and surgical site infection [7,14]. Experience with TOEPVA is limited in the literature. A series of 12 patients in Thailand by Sasanakietkul et al demonstrated the procedure’s safety when performing biochemical treatment of primary hyperparathyroidism, without significant complications [3]. Although traditional parathyroid surgery has low complication rates, a minimally invasive approach further decreases the risk of complications, but they still occur. Injury to the recurrent laryngeal nerve is a serious complication of endocrine surgery and has consequences of hoarseness or airway occlusion [15]. One transient recurrent nerve injury has been reported as an outcome consistent with focused surgery. In our series, temporary recurrent laryngeal nerve plasy was observed once, and hoarseness regressed during follow-up.
Topographically, a concordant imaging of hyperfunctioning parathyroid adenoma on Tc99m, MIBI scintigraphy, and ultrasonography/CT scan is essential before planning any focused or EP approaches for optimal outcome. Focused surgery was performed on the gland, which was localized preoperatively by scintigraphy and ultrasound and marked with methylene blue using ultrasound [16].
Another serious complication is permanent hypoparathyroidism. While transient hypocalcemia may account for up to 50% of patients undergoing parathyroidectomy, permanent hypoparathyroidism is quite rare and occurs in less than 1% of cases. As MIP techniques are generally utilized in cases of single adenoma removal, this complication is much less of a concern. Transient hypocalcemia was observed in 2 patients after classical surgery and 7 patients after TOEPVA [15].
Fernandez-Ranvier et al emphasized that complication rates were related to surgeon experience and decreased significantly after a surgeon had performed at least 12 operations [14]. IONM is also recommended in TOETVA. The present results show that it can be safely applied in experienced centers in terms of recurrent nerve injury in vestibular surgery.
New complications associated with transoral vestibular approach surgery include mental nerve injury, jaw flap perforation, and tearing of the oral commissure or lower labial frenulum. This is most common with robotic surgery. In all cases, the fact that the working space for the mouth was not narrowed by nasal intubation prevented commissure tears. We used a 10-mm initial horizontal incision at least 1 cm from the frenulum and did not encounter any frenular or commissural tears. The literature has documented a high complication rate (15.6–100%) for mental nerve injury using the robot-assisted technique due to 5-mm incisions close to the central incisions [17]. In our series, 5-mm vertical incisions were used to provide more lip mobility and reduce the tension of the mental nerve where it exits the mental foramen. Mental nerve damage was not observed in our series. Strict adherence to strict rules has prevented the occurrence of these complications.
According to previous studies, the incidence of hematoma is 0.5–1.6% [7]. Haematoma was not observed in our case series. In focused surgery, vicryl threads tie the vascular structures, whereas in TOEPVA careful dissection is performed using only energy-based devices.
Burning of the skin flap, which has been reported among other complications, can occur when applying the vestibular technique. No skin complications were observed in our series. In addition, the skin was kept wet during flap dissection, and hook cautery was used during flap preparation.
In the literature, no significant difference was found in the duration of hospitalization [18]. In our series, there was no difference in terms of length of hospitalization. Although the length of hospital stay is expected to be shorter in minimally invasive surgeries, the endoscopic vestibular approach is considered a nonscar surgery, not a minimally invasive surgery.
Operative times in TOEPVA varied widely in the studies reviewed. The results suggest that endoscopic procedures have longer operative times than the traditional open approach for reasons such as port placement and flap preparation [17]. The range of operative times in TOEPVA varies significantly among institutions, possibly due to surgeon experience and various other reasons. As experience increases, operative times decrease significantly, which is an expected result. Anuwong’s team in Thailand reported TOEPVA operative times comparable to the standard approach for primary hyperparathyroidism, at 107.5 min for the open approach and 144 min for TOEPVA [3]. In our series, the mean operative time was 80.54 min for open surgery and 128.21 min for TOEPVA. Although the unknown dissection line is shorter than other minimally invasive parathyroid techniques, it prolongs the operation time. In our TOEPVA series, the operation time for the first patient was 158 min, and it was 97 min for the last patient. Any newer procedure becomes easier with experience and the learning curve becomes flatter with time as the surgical team learns to deal with technical and ergonomical constraints [16].
The literature describes the conversion to open surgery in vestibular surgery mainly due to uncontrolled bleeding, air embolism, jawbone and difficult dissection area, and tracheal injury. In general, the endoscopic completion rate of the operation is 96% in highly experienced centers. The reasons for conversion to focused open surgery were generally described as uncontrollable bleeding and the difficulty of a narrow working field. The literature has also shown that advanced age and high BMI are risk factors for these complications. In our center, only 1 case was converted to open surgery due to bleeding, and this was the 3rd case of the series and was done to control bleeding after parathyroid removal [9,14].
The most significant advantage of TOEPVA is that it offers a “scarless” procedure (ie, without visible scarring) by hiding the incision in the mouth. While most patients are not overly bothered by the parathyroidectomy scar, the visible scar is an annoyance in daily life for some patients. Best et al surveyed patients more than 1 year postoperatively who had undergone mid-cervical thyroidectomy and found that 10.1% indicated they would consider scar revision in the future [19]. It has also been shown that patients with a traditional neck incision after focused parathyroidectomy are more likely to have chronic skin diseases such as psoriasis and severe atopic eczema, with a lower quality of life [20]. Today, increasing aesthetic concerns make surgical procedures with concealable scars attractive. In our study, the mean age of patients who chose the TOEPVA technique was considerably younger than that of patients who underwent focused surgery.
A study by Johns Hopkins University that recorded real-time eye fixations showed that the faces of patients who had undergone transoral surgery were indistinguishable from those of people who had not, even though open neck surgery scars distract attention from the face [21]. This is precisely what patients want. It is, therefore, prudent for surgeons to be able to offer TOEPVA to patients who wish to avoid any visible scaring, especially in younger and female populations. Although the initial costs of the transoral vestibular approach are high, the potential for increased cosmetic prospects, decreased pain, and improved quality of life should be considered in scarless neck surgery.
Inclusion and exclusion criteria for patient selection in TOEPVA may differ among institutions due to the lack of uniform standards. Patients with a history of thyroiditis, previous radiation therapy, or suspected malignancy should be excluded. The criteria for selection of patients for TOEPVA are as follows: no previous neck surgery, no history of head and neck radiation, no oral infection, no adenoma in the retrosternal region, no recurrent adenoma, no angled jaw anatomy, and for aesthetic purposes. These indications should be strictly followed. In the present study, the surgeon performing TOEPVA surgery attended hands-on cadaveric courses on TOEPVA before starting to complete the operating procedures.
According to the literature, endoscopic surgery experience and surgeon patience are crucial for successful TOEPVA surgery. The surgery should be performed by experienced surgeons trained in endoscopic surgery and TOEPVA. Selecting patients with BMI in the normal range for the first cases is recommended.
TOEPVA is in the Natural Orifice Surgery Group due to the need for more tissue dissection to reach a location away from the incision site. The transoral approach to thyroidectomy and parathyroidectomy is classified as ‘clean-contaminated’ surgery and inherently carries a higher risk of infection than clean transcervical thyroidectomy [22]. Moreover, only 1 neck infection (0.1%) has been reported. In our series, soft-tissue infection was observed in only 1 of our TOEPVA cases.
Persistent/recurrent hyperparathyroidism occurs in 2–5% of patients with sporadic primary hyperparathyroidism. The most common causes of persistent/recurrent hyperparathyroidism include unrecognized four-gland hyperplasia, ectopic location of the hyperfunctioning parathyroid gland(s), or operations performed by inexperienced or low-volume parathyroid surgeons. In our series of patients, no cases of persistent hyperparathyroidism were observed [9].
Compared to the focused open surgery approach, TOEPVA has longer operative times and higher operative costs. However, the use of focused open surgical equipment reduces the cost.
The main limitation of our study is that randomization was not possible because it was retrospective. Other limitations are the small number of cases and the fact that open surgery was not performed by a single physician.
Conclusions
No significant differences were found between the 2 techniques in terms of reliability and complication rates. TOEPVA is a surgical method that can be applied safely, especially in suitable patients who want to avoid visible scars on the neck.
Figures
 Figure 1. Position of incision for TOEPVA. The midline incision was created as a 10-mm incision just above the frenulum towards the oral vestibule. Other incisions were made with two 5-mm vertical incisions on the lateral aspect of the canines, almost at the level of the first molar.
Figure 1. Position of incision for TOEPVA. The midline incision was created as a 10-mm incision just above the frenulum towards the oral vestibule. Other incisions were made with two 5-mm vertical incisions on the lateral aspect of the canines, almost at the level of the first molar.  Figure 2. Posteoprative view of lip after TOEPVA. After controlling bleeding in the lip mucosa, the incisions were closed with 4/0 monocryl absorbable suture material.
Figure 2. Posteoprative view of lip after TOEPVA. After controlling bleeding in the lip mucosa, the incisions were closed with 4/0 monocryl absorbable suture material. 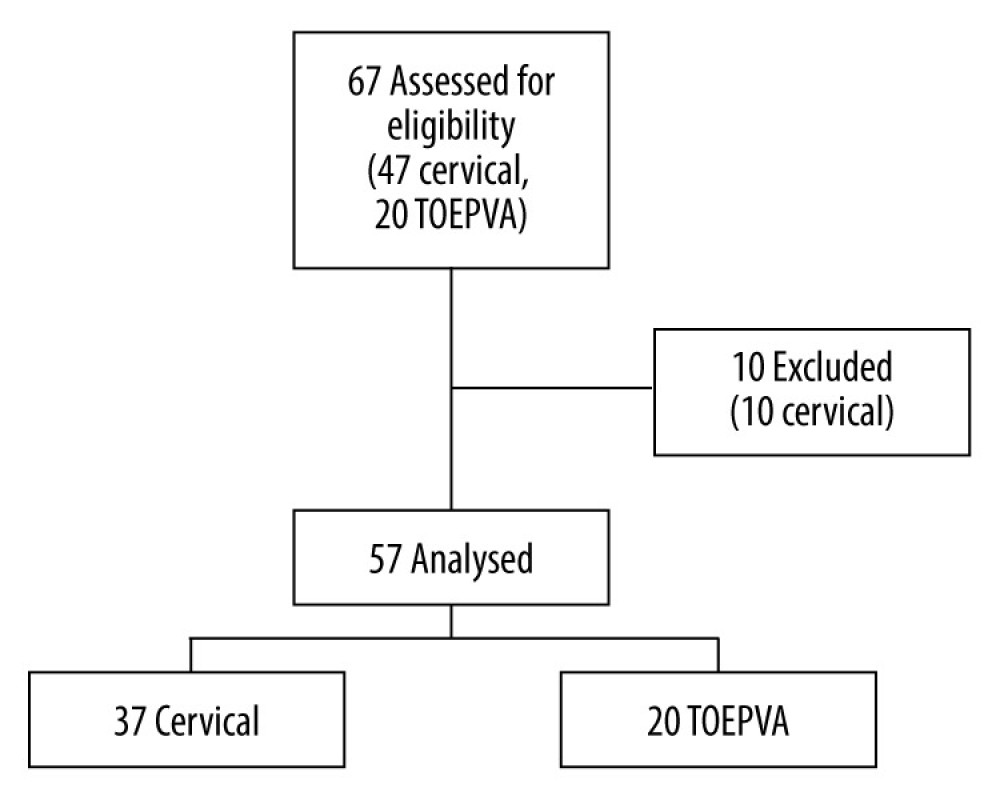 Figure 3. Analysis of total parathyroidectomies performed and included in the study.
Figure 3. Analysis of total parathyroidectomies performed and included in the study. 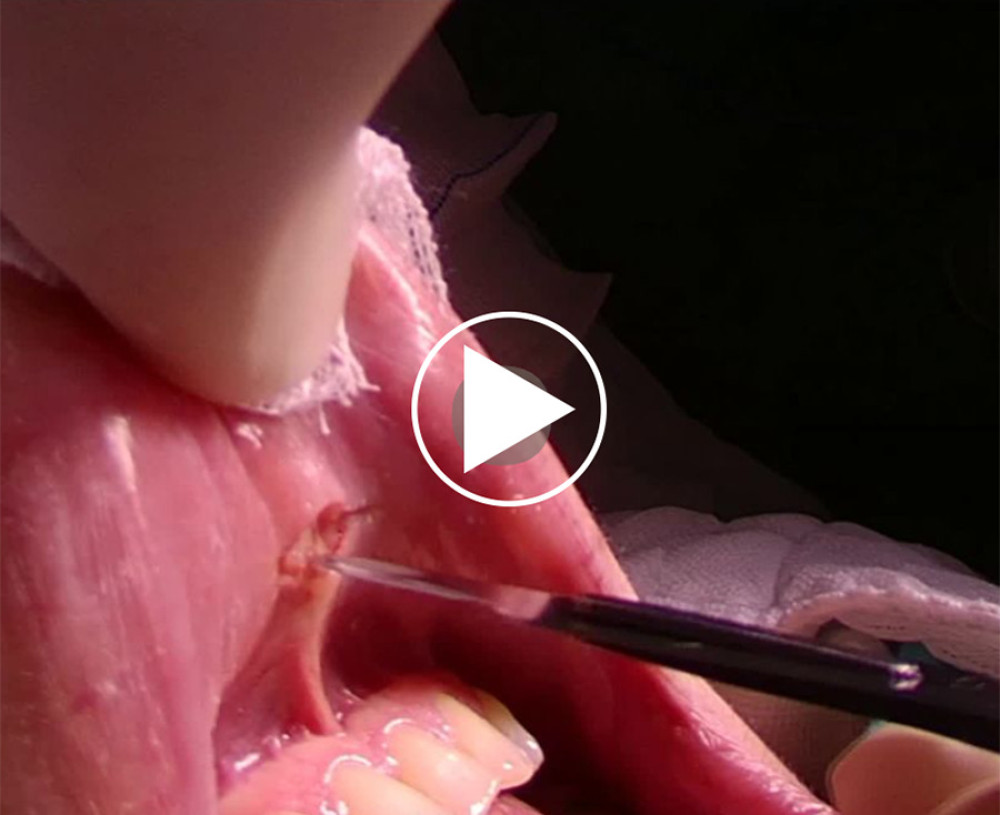 Video 1. Trocar placements were made after hydro dissection.
Video 1. Trocar placements were made after hydro dissection.  Video 2. Blunt and sharp dissections.
Video 2. Blunt and sharp dissections.  Video 3. The parathyroid tissue was localized and marked with Methylene blue.
Video 3. The parathyroid tissue was localized and marked with Methylene blue. References
1. Delbridge LW, Palazzo FF, First parathyroid surgeon: Sir John Bland-Sutton and the parathyroids: ANZ J Surg, 2007; 77(12); 1058-61
2. Bellantone R, Raffaelli M, DE Crea C, Minimally-invasive parathyroid surgery: Acta Otorhinolaryngol Ital, 2011; 31(4); 207-15
3. Sasanakietkul T, Jitpratoom P, Anuwong A, Transoral endoscopic parathyroidectomy vestibular approach: A novel scarless parathyroid surgery: Surg Endosc, 2017; 31(9); 3755-63
4. Udelsman R, Donovan PI, Sokoll LJ, One hundred consecutive minimally invasive parathyroid explorations: Ann Surg, 2000; 232(3); 331-39
5. Miura D, Wada N, Arici C, Does intraoperative quick parathyroid hormone assay improve the results of parathyroidectomy?: World J Surg, 2002; 26(8); 926-30
6. Hurtado-López LM, Gutiérrez-Román SH, Basurto-Kuba E, Luna-Ortiz K, Endoscopic transoral parathyroidectomy: Initial experience: Head Neck, 2019; 41(9); 3334-37
7. Anuwong A, Transoral endoscopic thyroidectomy vestibular approach: A series of the first 60 human cases: World J Surg, 2016; 40(3); 491-97
8. Chen S, Zhao M, Qiu J, Transoral vestibule approach for thyroid disease: A systematic review: Eur Arch Otorhinolaryngol, 2019; 276(2); 297-304
9. Wang Y, Ladie DE, Parathyroidectomy: StatPearls [Internet] Sep 26, 2022, Treasure Island (FL), StatPearls Publishing
10. Chai YJ, Kim HY, Kim HK, Comparative analysis of 2 robotic thyroidectomy procedures: Transoral versus bilateral axillo-breast approach: Head Neck, 2018; 40(5); 886-92
11. Dionigi G, Wu CW, Tufano RP, Monitored transoral endoscopic thyroidectomy via long monopolar stimulation probe: J Vis Surg, 2018; 4; 24
12. Navarra G, Bartolo V, Rizzo AG, Pre- and post-operative patient care for transoral thyroidectomy: Ann Thyroid, 2018; 3; 3
13. Barczyński M, Cichoń S, Konturek A, Cichoń W, Minimally invasive video-assisted parathyroidectomy versus open minimally invasive parathyroidectomy for a solitary parathyroid adenoma: A prospective, randomized, blinded trial: World J Surg, 2006; 30(5); 721-31
14. Fernandez Ranvier G, Meknat A, Guevara DE, International multi-institutional experience with the transoral endoscopic thyroidectomy vestibular approach: J Laparoendosc Adv Surg Tech A, 2020; 30(3); 278-83
15. Wolfe SA, Fingeret A, Parathyroid minimally invasive surgery: StatPearls [Internet] May 29, 2023, Treasure Island (FL), StatPearls Publishing
16. Bhargav PRK, Sabaretnam M, Amar V, Devi NV, Applicability of transoral endoscopic parathyroidectomy through vestibular route for primary sporadic hyperparathyroidism: A South Indian experience: J Minim Access Surg, 2019; 15(2); 119-23
17. Wilhelm T, Wu G, Teymoortash A, Transoral endoscopic thyroidectomy: Current state of the art – a systematic literature review and results of a bi-center study: Transl Cancer Res, 2016; 5; S1521-30
18. Anuwong A, Ketwong K, Jitpratoom P, Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach: JAMA Surg, 2018; 153(1); 21-27
19. Best AR, Shipchandler TZ, Cordes SR, Midcervical scar satisfaction in thyroidectomy patients: Laryngoscope, 2017; 127(5); 1247-52
20. Choi Y, Lee JH, Kim YH, Impact of postthyroidectomy scar on the quality of life of thyroid cancer patients: Ann Dermatol, 2014; 26(6); 693-99
21. Liao D, Ishii LE, Chen LW, Transoral neck surgery prevents attentional bias towards the neck compared to open neck surgery: Laryngoscope, 2020; 130(6); 1603-8
22. Makay Ö, Sabuncuoğlu MZ, Turan Mİ, Transoral endoscopic parathyroidectomy vestibular approach (TOEPVA) for primary hyperparathyroidism: Turkey’s experience: Surg Endosc, 2022; 36(2); 1037-43
Figures
 Figure 1. Position of incision for TOEPVA. The midline incision was created as a 10-mm incision just above the frenulum towards the oral vestibule. Other incisions were made with two 5-mm vertical incisions on the lateral aspect of the canines, almost at the level of the first molar.
Figure 1. Position of incision for TOEPVA. The midline incision was created as a 10-mm incision just above the frenulum towards the oral vestibule. Other incisions were made with two 5-mm vertical incisions on the lateral aspect of the canines, almost at the level of the first molar. Figure 2. Posteoprative view of lip after TOEPVA. After controlling bleeding in the lip mucosa, the incisions were closed with 4/0 monocryl absorbable suture material.
Figure 2. Posteoprative view of lip after TOEPVA. After controlling bleeding in the lip mucosa, the incisions were closed with 4/0 monocryl absorbable suture material.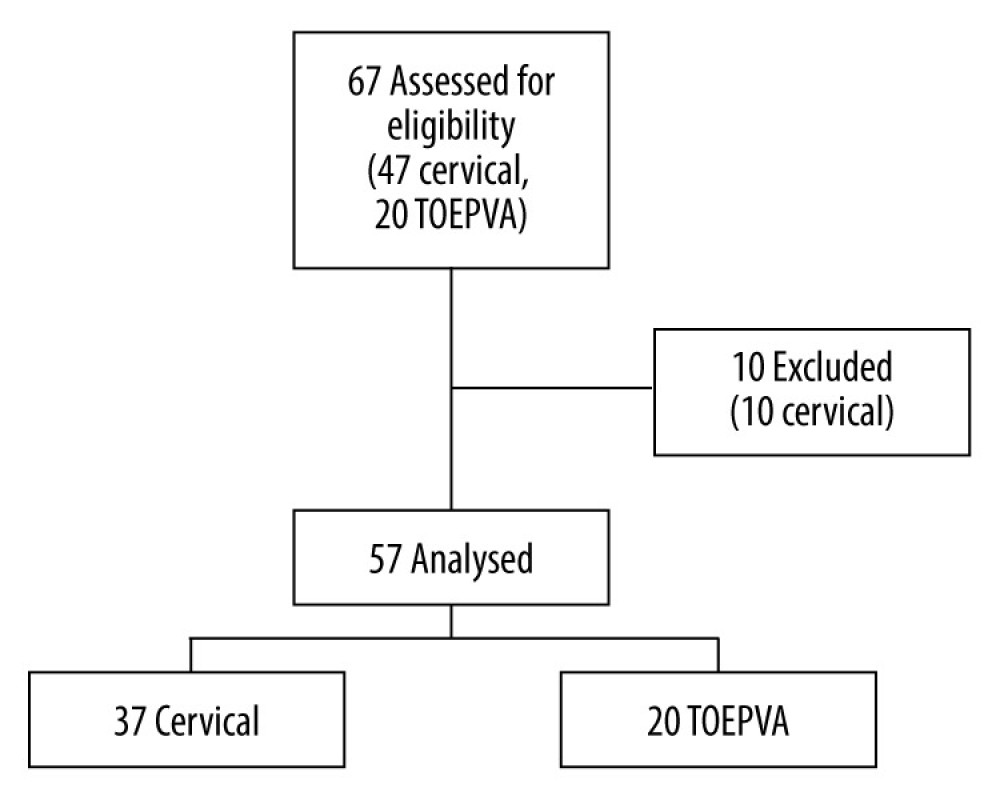 Figure 3. Analysis of total parathyroidectomies performed and included in the study.
Figure 3. Analysis of total parathyroidectomies performed and included in the study.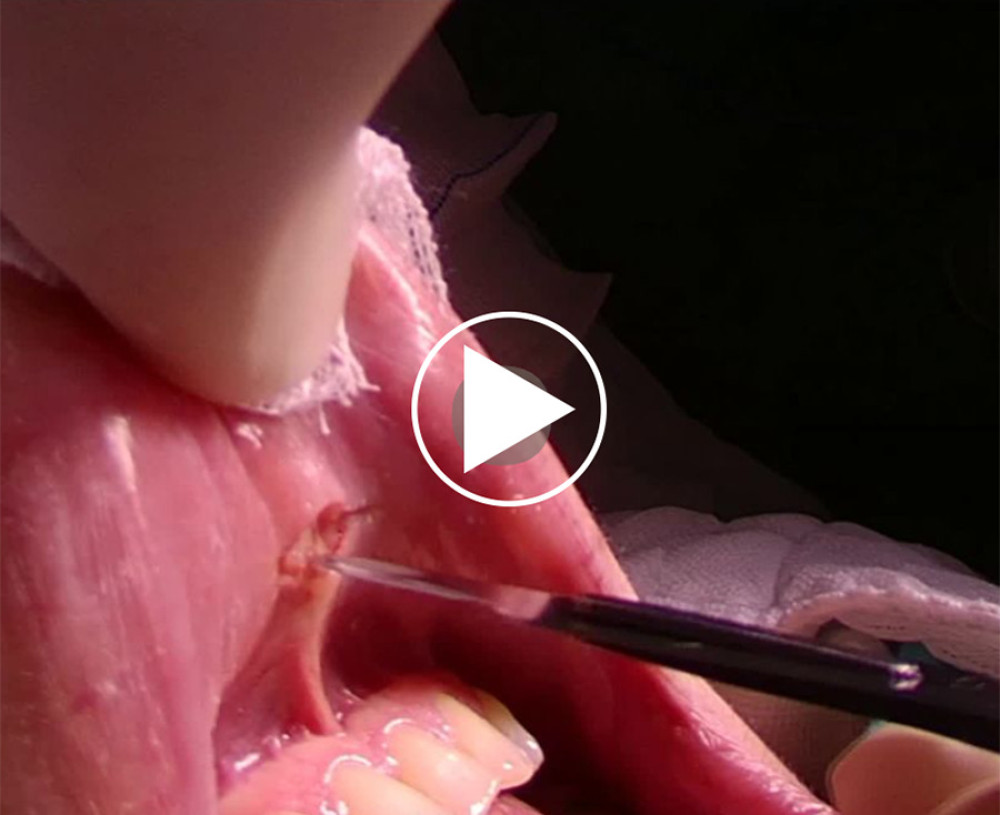 Video 1. Trocar placements were made after hydro dissection.
Video 1. Trocar placements were made after hydro dissection. Video 2. Blunt and sharp dissections.
Video 2. Blunt and sharp dissections. Video 3. The parathyroid tissue was localized and marked with Methylene blue.
Video 3. The parathyroid tissue was localized and marked with Methylene blue. In Press
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952