02 May 2024: Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff) and Eyelid (TOF Scan) Using Mivacurium during General Anesthesia
Paweł RadkowskiDOI: 10.12659/MSM.943630
Med Sci Monit 2024; 30:e943630
Abstract
BACKGROUND: Mivacurium is a non-depolarizing neuromuscular blocking agent. TOF-Cuff® is a device that monitors intraoperative neuromuscular blockade and blood pressure. TOF-Scan® measures muscle relaxation status of an anaesthetized patient. This study included 36 patients aged 18 to 75 years presenting for elective surgery, to compare neuromuscular blockade measured using the TOF-Cuff of the upper arm and the TOF-Scan of the facial corrugator supercilii muscle during general anesthesia and following administration of mivacurium.
MATERIAL AND METHODS: Train-of-four (TOF) values were obtained every 30 s before intubation and successively every 5 min until extubation.
RESULTS: The median onset time for TOF-Cuff was longer than for TOF-Scan (210 s vs 90 s, P<0.00001). Multiplying the time to relaxation (according to TOF-Scan) by 1 to 8, respectively, provided concordance with the TOF-Cuff result for the following cumulative percentages of patients: 5.5%, 38.9%, 58.3%, 77.8%, 83.3%, 86.1%, 88.9%, and 91.7%. Analogue values for time to recovery from the last dose were 11.1%, 63.9%, 83.3%, 86.1%, 86.1%, 88.9%, 88.9%, and 91.7%. The proportion of patients who still had TOFratio=0 in the assessment performed at min 15 did not differ significantly between these 2 methods (P=0.088). Both TOF-Scan and TOF-Cuff showed a false-negative result in patients with clinical symptoms of preterm recovery; the numerical difference favored TOF-Cuff (1.6% vs 2.1%) but without statistical significance (P=0.2235).
CONCLUSIONS: When measurement on the limb is not possible, TOF-Scan on the eyelid can be an alternative for TOF-Cuff on the upper arm, if the time to relaxation is multiplied by at least 8, which is enough for 90% of patients.
Keywords: Equipment and Supplies, Intubation, Neuromuscular Monitoring, extubation
Introduction
Ulnar nerve palm mechanometry was previously the criterion standard for measuring muscle relaxation during general anesthesia in clinical trials, and is now receiving renewed interest [1]. The prevailing clinical norm for neuromuscular monitoring involves acceleromyography [2]. The response of the adductor pollicis muscle to electrical stimulation of the ulnar nerve is clinically used as a routine method of monitoring neuromuscular blockade [3]. Typically, an electrical stimulus is applied through adhesive electrodes positioned on the medial lower arm over the ulnar nerve to elicit nerve stimulation, for example, with the TOF-Scan®; the resultant motor response is quantified in terms of acceleration [4]. The frequently used paradigm is the train-of-four (TOF), in which the motor responses from the fourth and first stimuli are compared and presented as a percentage, denoted as the TOF ratio (TOFratio) [4].
In some patients, however, relaxometry on the hand is not possible, specifically for patients with fractures of the arms on both sides, burns of both forearms, amputations, and malformations of the upper extremities, and for those patients whose both arms must be fixed during surgery or for whom access is difficult. For these patients, facial nerve relaxometry is an alternative.
In facial nerve stimulation, the orbicularis oculi muscle around the eye, which has a typical muscular response of eyelid closing, and the corrugator supercilii muscle, which has a typical muscular response of eyebrow wrinkling, are more resistant to neuromuscular conduction blocking agents than is the adductor pollicis muscle; this resistance can result in neuromuscular conduction blockade overdose and a longer recovery rate [3,5]. The orbicularis oculi muscle and corrugator supercilii muscle respond to neuromuscular blockers with different sensitivity. Some studies suggest that the corrugator supercilii is a good predictor of laryngeal and diaphragmatic muscle relaxation [5,6]. However, there is a difference in the responding muscles depending on the neuromuscular blocker administered. Onset time (time from neuromuscular conduction blocking agent to TOFratio of 0%) after rocuronium administration corresponds to laryngeal and diaphragmatic muscles, but after mivacurium administration there are significant differences between onset time in the supraglottic muscles and laryngeal and diaphragmatic muscles [5–8].
A new neuromuscular monitoring device, the TOF-Cuff®, has been adopted as a new routine for monitoring the effects of neuromuscular activity [9,10]. The device is a modified blood pressure cuff with integrated electrodes for brachial plexus stimulation [9,10]. The TOF-Cuff device is therefore a compressomyograph, with which neuromuscular blockade is assessed by analyzing pressure changes produced by muscular activity within the cuff after peripheral nerve stimulation at the upper arm [2].
Studies show that there is compatibility between the TOF-Cuff and standard neuromuscular monitors (eg, TOF-Watch and TOF-Scan) that use acceleromyography of the adductor pollicis. However, the TOFratio does not respond during the recovery phase [2,9,11].
Mivacurium is a nondepolarizing neuromuscular blocking drug with the shortest duration of action and the fastest rate of recovery (due to rapid elimination by cholinesterase) but with a longer onset time [12]. Mivacurium competitively binds to cholinergic receptors on the motor end-plate, counteracting the effects of acetylcholine and leading to the inhibition of neuromuscular transmission. This agent is used as a supplement to general anesthesia to induce skeletal muscle relaxation and facilitate endotracheal intubation and mechanical ventilation [12]. Good intubating conditions are reached after 2 to 3 min, and recovery time to more than 75% TOF is 29.5 to 32.1 min at a dose of 0.20 mg/kg of mivacurium [13].
This is the first study that compares the TOF-Scan on the corrugator supercilii and TOF-Cuff on brachial muscles with the administration of mivacurium. We hypothesized that there are no statistically significant differences between the 2 neuromuscular monitors. Therefore, this study included 36 patients between 18 to 75 years of age presenting for elective surgery, to compare neuromuscular blockade measured using the TOF-Cuff of the upper arm and the TOF-Scan of the facial corrugator supercilii muscle during general anesthesia and following administration of mivacurium.
Material and Methods
ETHICAL APPROVAL:
This prospective, observational clinical trial was approved by the Bioethics Committee at the Faculty of Medicine of the Medical College of the University of Warmia and Mazury in Olsztyn (No. 10/2021) and registered at
STUDY DESIGN:
To find a difference of about 30 s with a 60 s standard deviation (alpha=0.05, power=0.80;
ANESTHETIC PROCEDURES:
Anesthetic management was standard for all patients. Monitoring included an electrocardiogram, noninvasive blood pressure TOF-Cuff (Viridian Poland) placed on the opposite side of the intravenous line, pulse oximetry (Dräger), and capnography (Dräger). The TOF-Scan (Dräger) device was placed over the eyelid. Two electrodes were attached to the temporal branch of the facial nerve at a point in front of the earlobe, and the amplitude of the 4-string stimulus was set at 40 mA (Figure 1A). The TOF-Cuff was placed on the upper extremities after careful skin preparation and positioning, according to the manufacturer’s instructions, right next to the brachial muscles, and the amplitude of the TOF stimulus was set at 40 mA (Figure 1B). Anesthesia was induced with fentanyl (Polpharma), propofol (Fresenius Kabi), lidocaine (Polpharma; if no epidural was used), dexamethasone (Bausch Health), and mivacurium (Aspen Pharma) at a dose of 0.2 mg/kg. Anesthesia was maintained with sevoflurane (Baxter Polska), with a minimal alveolar concentration of 1.0. The indication for intubation was a TOFratio of 0 on the TOF-Cuff. Physicians were able to administer additional doses of mivacurium to achieve complete spontaneous neuromuscular recovery after surgery. Hypotension was treated with ephedrine (Polpharma) or a fluid bolus, as clinically indicated. Hypertension was treated by increasing sevoflurane. Additional doses of fentanyl were administered as needed. Ventilation was controlled, and end-expiratory carbon dioxide values were maintained between 35 and 45 mm Hg. Ondansetron (Fresenius Kabi) was administered 30 min before the end of surgery. Neostigmine (Teva Pharmaceuticals Polska) at a dose of 40 μg/kg and atropine at a dose of 8 μg/kg were administered at the end of surgery to ensure complete recovery of neuromuscular function in patients who potentially failed to return spontaneously to a TOFratio≥0.9.
MEASUREMENTS:
After the patient lost consciousness and the administration of mivacurium was terminated, we started simultaneous TOFratio measurements on the supraspinatus muscle and arm every 30 s; after reaching 600 s, measurements were repeated every 5 min. The TOFratio was recorded, as well as the time of intubation, time of extubation, added dose of mivacurium, clinical signs of neuromuscular return, and adverse events. Intubation was rated by the clinician who performed the intubation on a scale of 1 (very easy) to 4 (very difficult). We assumed that onset time was the time between the end of mivacurium administration to TOFratio=0.
STATISTICAL ANALYSIS:
Due to the lack of normal distribution (assessed by the Shapiro-Wilk test), the distribution of continuous variables was presented as the median, interquartile range, and range. Regarding the dual measurement of the same patients using 2 methods, the Wilcoxon test was used to assess differences between them. TOFratio=0 was not reached in 3 patients; thus, the time to TOFratio=0 for both methods was illustrated using Kaplan-Meier curves and compared using the log-rank test.
To estimate the correction needed for TOF-Scan, the ratio of the time measured by both methods, TOF-Scan and TOF-Cuff, was calculated, and its distribution was presented using descriptive statistics. The relationship between continuous variables was assessed using the Spearman correlation coefficient. The difference between clinical symptoms of neuromuscular return and measurement results is presented as frequency and percentage. The significance of differences in the number of false negative measurements between the 2 measurement methods was evaluated using the chi-square test. Statistical analysis of the test results was performed in Statistica 13.3 (Tibco). The results were considered statistically significant at
Results
STUDY POPULATION:
Thirty-eight patients participated in the study. Two patients were excluded because their BMI values were too high. Ultimately, 36 patients were included in the analysis (2 [5.6%] men, 34 [94.4%] women), at the median (IQR, range) age of 52.5 years (40–64, 27–74) and BMI 24.25 (22.2–28.4, 18.1–33.95). Thirteen (36.1%) patients were classified at ASA stage I, 17 (47.2%) were at ASA II, and 6 (16.7%) at ASA III. During the study, patients underwent surgery in the following areas: 30 (83.3%) in gynecology, 2 (5.6%) in general surgery, 2 (5.6%) in orthopedics, 1 (2.75%) in ear-nose-throat, and 1 (2.75%) in vascular surgery. Most intubations (28 [77.8%]) were rated as very easy, 5 (13.9%) as easy, and 3 (8.3%) as rather difficult; there was no intubation rated as very difficult or not possible to perform. There were 5 adverse reactions: 4 cases of temporary redness of the skin of the face, neck, and chest, and 1 bronchospasm; 4 patients were intubated despite TOFratio>0 assessed with TOF-Cuff. Lidocaine was administered in 23 cases, epidural anesthesia in 7 cases, and no lidocaine or epidural was administered in 6 cases due to lack of indications or when there were contraindications to their use. In 3 patients, muscle block antagonists had to be used.
TIME TO ONSET:
In the time-to-event (onset) analysis, median time of onset of forearm muscle blockage was 210 s, while that of the supraspinatus muscle was 90 s (P<0.0000; Figure 2A). Three (8.3%) patients did not reach neuromuscular blockade after 600 s, becoming censored observations.
We did not demonstrate a significant Spearman correlation between the time to onset in TOF-Cuff measurements and the time to onset in TOF-Scan measurements. The lack of normal distribution precluded the use of Pearson correlation, which also ruled out the possibility of calculating a correction using linear regression. Therefore, we expressed the relationship between the results as the ratio of both measurements. In Table 1, we present the time-to-event ratio measured by the 2 methods, showing what proportion of the time to onset measured with TOF-Cuff is represented by the time to onset measured with TOF-Scan, and therefore by how much the time to onset measured with TOF-Scan needed to be multiplied to obtain a result similar to that measured with TOF-Cuff. The minimum value, successive deciles, and maximum for this correction factor were, respectively: 0.83, 1.5, 1.7, 2.0, 2.2, 3.0, 3.2, 3.5, 4.3, 6.5, and 8.0. The Bland-Altman plot is presented in Figure 2B.
The ease of intubation was not correlated with any demographic variable or with any variable assessing the time to relaxation.
RELAXATION TIME:
Out of 36 patients, only 4 received a single dose of mivacurium, while 32 (88.9%) received up to 10 additional doses (with the first additional dose administrated usually in minute 15). In the group of these 4 patients who received only 1 dose, the relaxation times according to the TOF-Cuff vs TOF-Scan method were as follows: 3.5 vs 8.0 min, 37.5 min vs 47.0 min, 3.5 min vs 54.0 min, and 27 min vs 19 min. The median value was 15.5 min vs 32 min. Due to the small sample size, we refrained from calculating quartiles and did not evaluate this difference with a statistical test.
When monitoring resumed at min 15, TOFratio=0 according to TOF-Cuff persisted in 17 patients (47.2%) who had not received an additional dose of mivacurium earlier, and in 23 (63.9%) among these patients according to TOF-Scan. A concordant result of TOFratio>0 according to both methods was achieved in 3 patients (11.1% of the total patients who did not receive an additional dose in the meantime), a concordant result of TOFratio=0 was obtained in 16 patients (59.3%), in 7 patients (26.0%) a result of TOFratio>0 was obtained only according to TOF-Cuff, and in 1 patient (3.7%) a result of TOFratio>0 was obtained only according to TOF-Scan. The difference in distribution was not statistically significant (
TIME TO RECOVERY:
The time from the last dose of mivacurium to TOFratio>90 was shorter for the supraspinatus muscle than for the forearm muscle (median 35 min [25–45 min, 15–90 min] vs 17.5 min [10–25 min, 0–80 min], P=0.000008). Figure 3 shows the Bland-Alttman plot. The Spearman correlation coefficient for time to recovery assessed with both methods was 0.4 (P<0.05); the sensitivity analysis revealed no influence of outlier observations; after excluding these observations, R equaled 0.43 (P<0.05). Time to recovery according to TOF-Cuff was not dependent on age, BMI, or ASA stage; however, it was dependent on time to onset according to TOF-Cuff (R=0.4, P<0.05) and relaxation time after the first dose (R=0.39, P<0.05). Time to recovery according to TOF-Scan was also not dependent on age or BMI but was dependent on time to onset, according to TOF-Scan (R=−0.37, P<0.05) and relaxation time after the first dose (R=0.37, P<0.05).
Similar to time to onset, we have presented the time to muscular return ratio (Table 2). The minimum value, successive deciles, and maximum for the correction factor were, respectively, 0.43, 1.0, 1.25, 1.5, 1.7, 1.8, 2.0, 2.2, 2.5, 3.5, and 10.
CLINICAL SIGNS OF PRETERM NEUROMUSCULAR RETURN:
Among 16 patients (44.4%), a total of 36 incidents were recorded that prompted the administration of an additional 2 mg of mivacurium based on the operator’s or anesthesiologist’s decision, due to the premature occurrence of own breathing, muscle tension, pushing, or movement (Table 3). During these 36 incidents, both methods yielded a false-negative result (TOFratio=0) in 16 cases (44.0%), both gave a correct result (TOFratio>0) in 7 cases (19.0%), only TOF-Scan provided an incorrect result in 9 cases (25.0%), and only TOF-Cuff in 4 cases (11.0%). Overall, TOF-Cuff indicated an erroneous result in 20 incidents (55.6%) and a correct result in 16 incidents (44.4%), while TOF-Scan produced an erroneous result in 25 incidents (69.4%) and a correct result in 11 incidents (30.6%). This difference was not statistically significant (P=0.2235). In the whole study group, a total of 1202 assessments were made for each method from intubation to extubation, indicating a minimal percentage of false-negative indications in both cases (1.6% and 2.1%) of all measurements conducted between intubation and extubation.
Discussion
In the present study, we demonstrated that, in adults, electrical stimulation of the facial nerve in the corrugator supercilii muscle using acceleromyography results in a significantly faster onset and recovery time after mivacurium, compared with that of brachial plexus nerves using compressomyography. In most studies, it was found that mivacurium had an average onset time of 150 to 240 s [13,14]. Statistical analysis in our study showed that TOFratio=0 on the arm occurred, on average, after 210 s, and on the eye, on average, after 90 s. The analysis also revealed a shorter time at which TOFratio=0 occurred, compared with the forearm muscles and corrugator supercilii.
Most studies had a similar onset time on the adductor pollicis, compared with our results on the arm muscles, as noted during the introduction of the TOF-Cuff, which is similar to the adductor pollicis [5,9,10,15–18]. However, compared with other studies, we obtained a shorter onset time in the corrugator supercilii muscle [5,18–21]. This may be related to the placement of the accelerometer or lack of calibration. The onset time on forearm muscles was longer than the onset time on the corrugator supercilii in our work and that of Hemmerling et al and Plaud et al [5,18]. This difference could be explained by the distinction between muscle fibers in forearm muscles and corrugator supercilii.
Laryngeal muscle block is crucial for intubation conditions. Several studies, conducted between 1996 and 2003, showed that the onset time of action of mivacurium on laryngeal muscles was shorter than that on buccal adductor muscles [5,18,21,22]. This has not yet been studied for forearm muscles. Values measured by acceleromyography on the supraspinatus muscle indicate an earlier possibility of intubation. However, our study does not provide data on the intensity of laryngeal muscle relaxation for adequate intubation conditions. Although the intensity of laryngeal muscle relaxation correlates with a lack of response from the eye muscles, it is important to note that, in a 1997 study, Patel et al found that the administration of a total of 0.25 mg of mivacurium for intubation after a 90-s optimal condition for intubation was not achieved in 10 of 16 patients [23].
Compared with earlier clinical studies, which were conducted on smaller study collectives (maximum 20 patients), our investigation included 32 patients. The results of our study provide new insights into the use of mivacurium with the TOF-Cuff. Much larger studies were performed by Honing et al (n=250) [24], who observed the difference between the compressomyography at the upper arm and electromyography at the adductor pollicis. In that study, the TOF-Cuff overestimated spontaneous neuromuscular block recovery, probably due to the use of a different neuromuscular blocking agent (rocuronium instead of mivacurium) in a different population than ours (involving patients with obesity, who were excluded in our study) and monitoring the different muscle. Krijtenburg et al [25], who compared these 2 methods after administration of rocuronium in 30 patients, also observed longer (average: 25 min) time to recovery in acceleromyography and electromyography measurements than in TOF-Cuff method. In contrast to mivacurium, which is a short-acting nondepolarizing neuromuscular relaxant but of slower onset of action, rocuronium has a rapid onset but with intermediate duration of action [26]. The response of different muscles to various drugs varies [27]; therefore, when administering corrections to patients requiring a TOF-Scan due to their clinical condition, special attention should be paid to the type of muscle relaxant used.
In our study, 3 patients did not achieve a decrease of TOFratio to 0 on the forearm muscles. Despite this, in the case of 2 patients, intubations were performed with ease, rated 1 on the difficulty scale, while in the other patient, intubation was assessed at 3 on the difficulty scale. However, in those cases, we achieved TOFratio=0 on the corrugator supercilii, which could correlate with variable muscle sensitivity to mivacurium in the specific bias. In our study, the ease of intubation was not correlated with any variable assessing the time to relaxation.
According to the “Guidelines on muscle relaxants and reversal in anesthesia” proposed by Plaud et al, monitoring of relaxation of the corrugator supercilii muscle can be used to decide when to perform tracheal intubation, because the corrugator supercilii muscle has similar sensitivity to neuromuscular blocking agents as the laryngeal muscles [8,28]. However, in the study by Dieck et al, only 20% of patients had optimal intubating conditions after using mivacurium, despite the authors waiting more than 3 min to intubate [16]. Similar recommendations were formulated in the guidelines of the British Association of Anaesthetists for the year 2021, which state, “The ulnar nerve is the most useful site for neuromuscular monitoring. However, if thumb movement is impeded, for example, when the hand is inaccessible during surgery, readings may be unreliable especially when acceleromyography devices are used. Alternative options include the use of electromyography devices, a compressomyography device such as the TOF-Cuff (Gwenagen Ltd, Leeds, UK) or use of alternative sites such as the facial or tibial nerve” [29].
Our data suggest that the corrugator supercilii muscle should not be used routinely to monitor the recovery phase of mivacurium block, because the corrugator supercilii muscle has similar sensitivity to the laryngeal muscles, and the laryngeal muscles recover faster than the pharyngeal and tongue muscles. Thilen et al revealed a 5-fold risk of postoperative residual curarization when monitoring the facial muscles [27,30]; to reduce this risk, the authors of recommendations cited above suggest stimulating ulnar nerve at the end of surgery [29]. Despite these reservations, it can be cautiously suggested that the corrugator supercilii muscle can serve as a clinically useful alternative when the upper limb is not readily available if an anesthesiologist keeps in mind the need of proper correction. Nevertheless, further studies with other muscle relaxants are needed to determine whether the corrugator supercilii muscle acceleromyography provides an accurate assessment of neuromuscular function under general anesthesia. So far, to the best of our knowledge, a similar study using different neuromuscular blocking agents has been conducted only by Chau et al, who assessed both methods after the administration of atracurium, obtaining similar results to ours [31].
Our study has several limitations. First, only 3 patients in our study received muscle relaxant reversal drugs. A repeat study with randomization and systemic administration of muscle relaxant reversal drugs would be necessary to confirm our results. Second, due to the variety of procedures and operators performing them, our patients required different levels of neuromuscular blockade, which meant that our patients received a different number of doses of mivacurium. Third, during the study, we did not randomize the dominant and non-dominant half of the body. However, based on the clinical trial conducted by Claudius et al, this is of minimal importance, as no significant differences in neuromuscular response were observed between the 2 arms [32]. Fourth, it can also be a limitation that the study was conducted by physicians with different levels of experience; the team consisted of both an anesthesiology specialist and an anesthesiology resident physician. Fifth, children and patients over the age of 75 were not included in the study. Sixth, the presented Bland-Altman plots should be interpreted with caution, as the distribution of differences was at the borderline of significance regarding departure from the normal distribution (
Conclusions
Our study demonstrated the effectiveness of monitoring neuromuscular conduction using the TOF-Cuff on the upper arm muscles, compared with acceleromyography on the eye muscles. Our findings revealed a faster onset and recovery time in the corrugator supercilii muscle, with no significant differences in the percentage of indications inappropriate relative to clinical symptoms; additionally, there were no differences in the percentage of patients in whom the blockade persisted at min 15. Despite faster onset and return, this method can be considered as a potential alternative when upper limb monitoring is impossible or contraindicated. Our results can help introduce necessary correction to adjust clinical decisions; the proposed corrections, however, are of a preliminary nature and require validation on a larger and more diverse population.
Figures
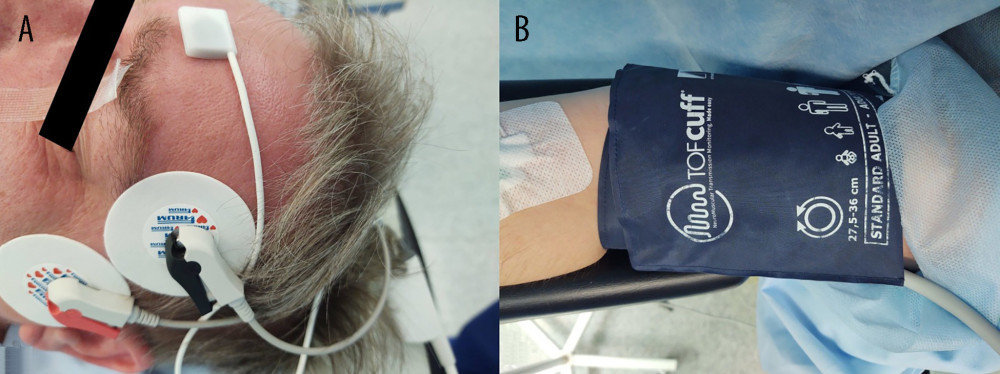 Figure 1. Placement of devices (A) TOF-Scan and (B) TOF-Cuff.
Figure 1. Placement of devices (A) TOF-Scan and (B) TOF-Cuff. 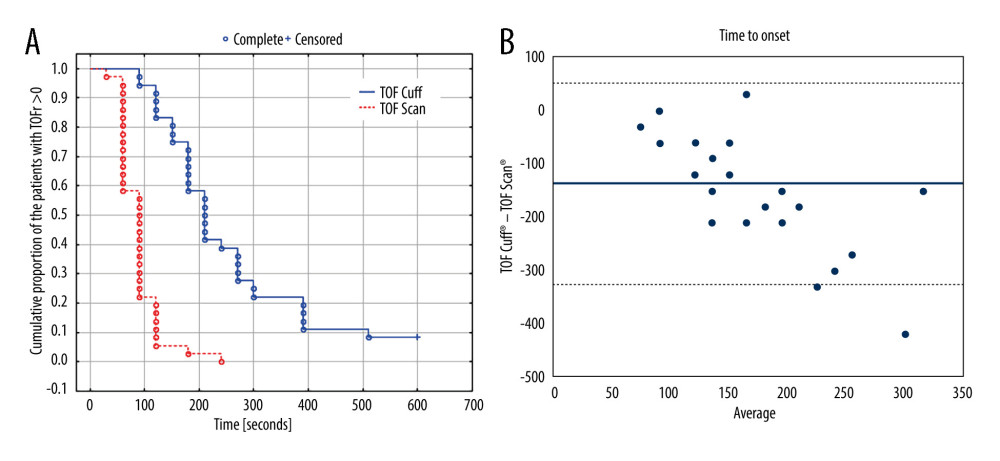 Figure 2. (A) Kaplan-Meier curve presenting time to TOFratio=0 measured with both methods. (Created in: Statistica 13.3, Tibco). (B) The Bland-Altman plot (average vs difference) for onset of neuromuscular block after mivacurium 0.2 mg/kg. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. (Created in: Microsoft Excel 2019). TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle.
Figure 2. (A) Kaplan-Meier curve presenting time to TOFratio=0 measured with both methods. (Created in: Statistica 13.3, Tibco). (B) The Bland-Altman plot (average vs difference) for onset of neuromuscular block after mivacurium 0.2 mg/kg. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. (Created in: Microsoft Excel 2019). TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle. 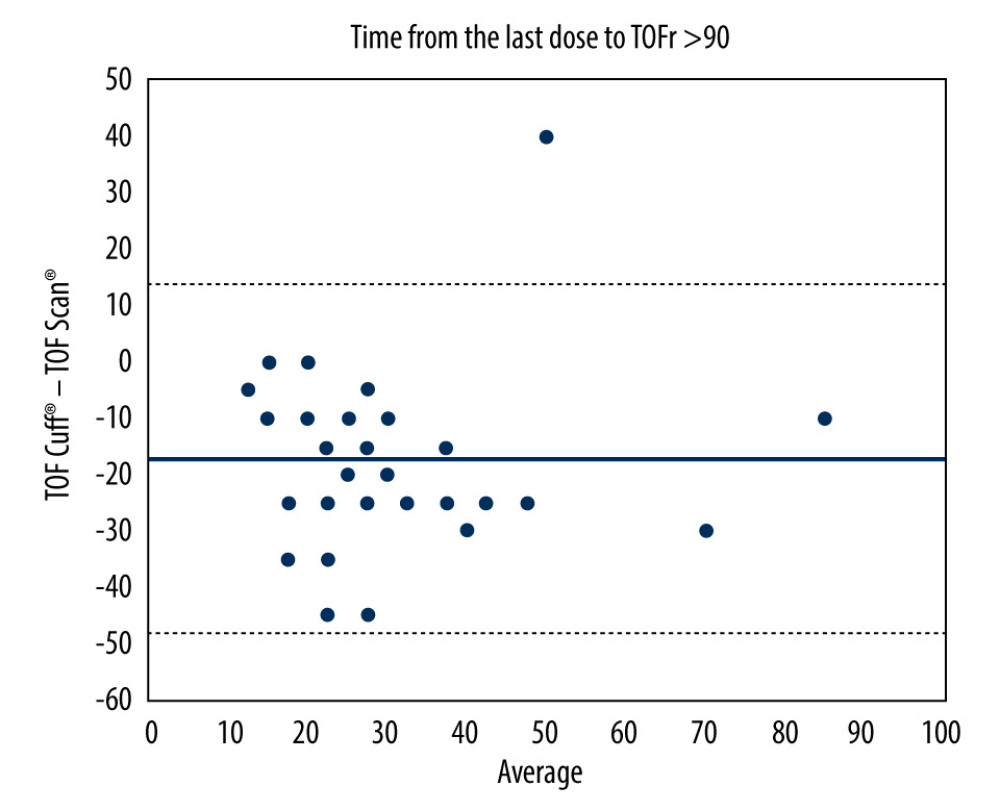 Figure 3. The Bland-Altman plot (average vs difference) for time from the last dose of mivacurium to TOFratio>90. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle. (Created in: Microsoft Excel 2019).
Figure 3. The Bland-Altman plot (average vs difference) for time from the last dose of mivacurium to TOFratio>90. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle. (Created in: Microsoft Excel 2019). Tables
Table 1. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time to TOFratio=0 measured by TOF-Scan against the same time measured by TOF-Cuff. Table 2. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time from the last 2 mg mivacurium dose to TOFratio>90 measured by TOF-Scan against the same time measured by TOF-Cuff.
Table 2. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time from the last 2 mg mivacurium dose to TOFratio>90 measured by TOF-Scan against the same time measured by TOF-Cuff.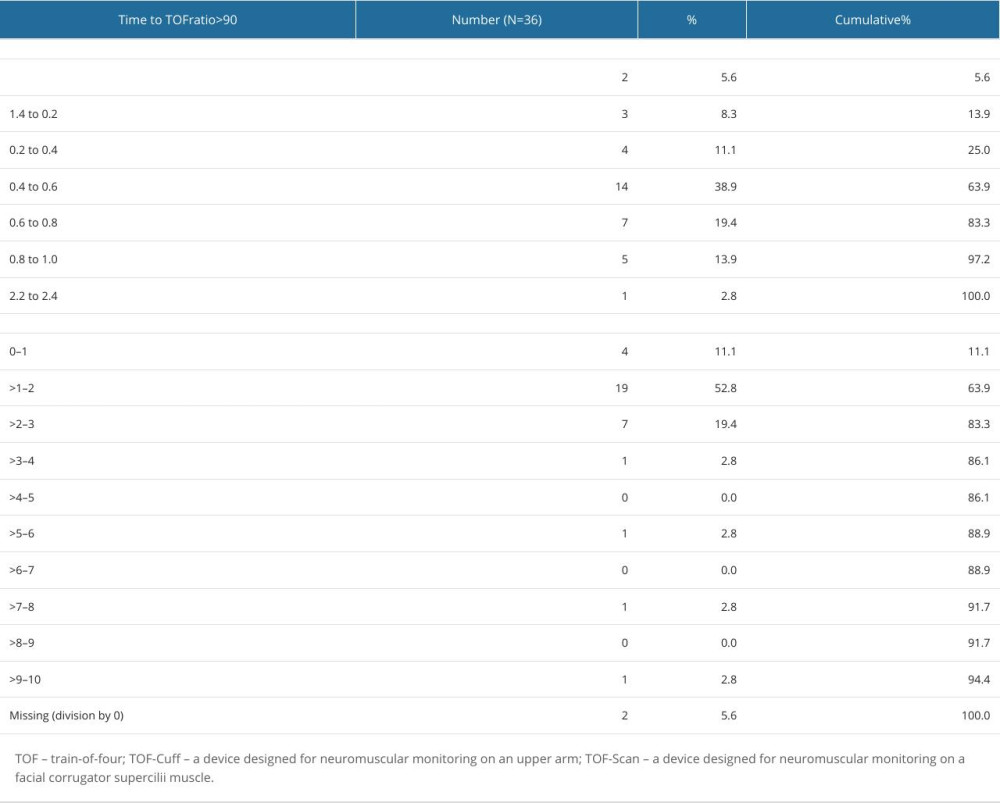 Table 3. Results of TOF (train-of-four) ratio measured with TOF-Cuff and TOF-Scan devices in patients with symptoms resulting in an additional dose of 2 mg mivacurium.
Table 3. Results of TOF (train-of-four) ratio measured with TOF-Cuff and TOF-Scan devices in patients with symptoms resulting in an additional dose of 2 mg mivacurium.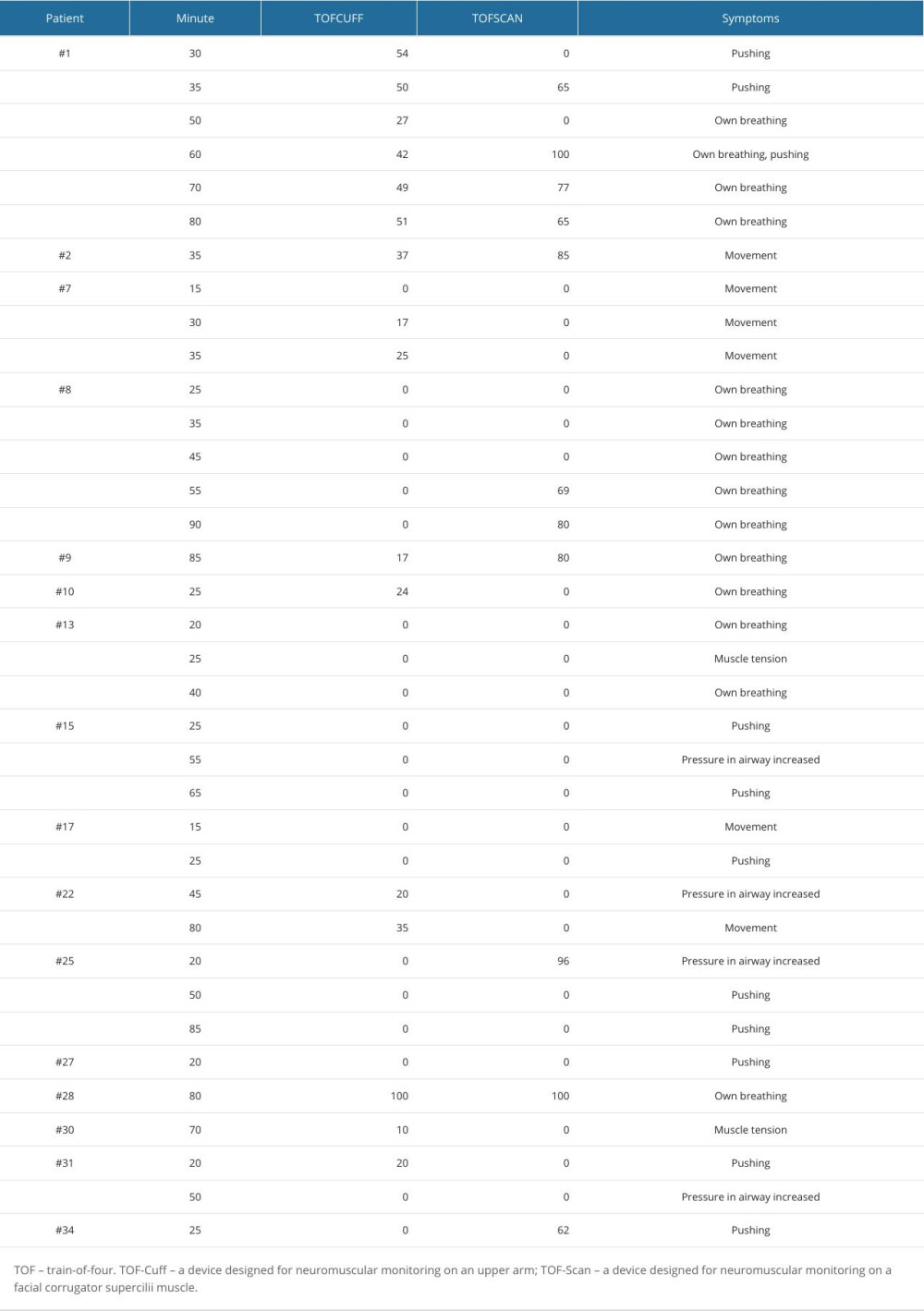
References
1. Lee W, The latest trend in neuromuscular monitoring: Return of the electromyography: Anesth Pain Med (Seoul), 2021; 16(2); 133-37
2. Murphy GS, Szokol JW, Avram MJ, Comparison of the TOFscan and the TOF-Watch SX during recovery of neuromuscular function: Anesthesiology, 2018; 129(5); 880-88
3. Naguib M, Brull SJ, Kopman AF, Consensus statement on perioperative use of neuromuscular monitoring: Anesth Analg, 2018; 127(1); 71-80
4. Markle A, Horn K, Welter J, Dullenkopf A, An observational study comparing the performance of TOF-Cuff with TOF-Scan monitoring during anaesthetic induction in clinical routine: Anaesthesiol Intensive Ther, 2020; 52(3); 181-86
5. Hemmerling TM, Schmidt J, Hanusa C, Simultaneous determination of neuromuscular block at the larynx, diaphragm, adductor pollicis, orbicularis oculi and corrugator supercilii muscles: Br J Anaesth, 2000; 85(6); 856-60
6. Hemmerling TM, Donati F, Neuromuscular blockade at the larynx, the diaphragm and the corrugator supercilii muscle: A review: Can J Anesth, 2003; 50(8); 779-94
7. Kirov K, Motamed C, Ndoko SK, Dhonneur G, TOF count at corrugator supercilii reflects abdominal muscles relaxation better than at adductor pollicis: Br J Anaesth, 2007; 98(5); 611-14
8. Plaud B, Debaene B, Donati F, The corrugator supercilii, not the orbicularis oculi, reflects rocuronium meeting abstracts at the laryngeal adductor muscles: Anesthesiology, 2001; 95(1); 96-101
9. Sfeir Machado E, Keli-Barcelos G, Dupuis-Lozeron E: Acta Anaesth Scand, 2020; 64(2); 173-79
10. Veiga Ruiz G, García Cayuela J, Orozco Montes J, Monitoring intraoperative neuromuscular blockade and blood pressure with one device (TOF-Cuff): A comparative study with mechanomyography and invasive blood pressure: Rev Esp Anestesiol Reanim, 2017; 64(10); 560-67
11. Kameyama Y, Takagi S, Seto K, Efficiency of the TOF-CuffTM for the evaluation of rocuronium-induced neuromuscular block and its reversal with sugammadex: A comparative study vs acceleromyography: J Anesth, 2019; 33(1); 80-84
12. Frampton JE, McTavish D, Mivacurium. A review of its pharmacology and therapeutic potential in general anaesthesia: Drugs, 1993; 45(6); 1066-89
13. Savarese JJ, Ali HH, Basta SJ, The clinical neuromuscular pharmacology of mivacurium chloride (BW B1090U). A short-acting nondepolarizing ester neuromuscular blocking drug: Anesthesiology, 1988; 68(5); 723-32
14. Larsen R, Annecke T, Fink T: Anestezjologia Part 1. The 4th Polish edition, 2020, Wrocław, Edra Urban & Partner
15. Abdulatif M, el-Sanabary M, Blood flow and mivacurium-induced neuromuscular block at the orbicularis oculi and adductor pollicis muscles: Br J Anaesth, 1997; 79(1); 24-28
16. Dieck T, Steffens J, Sander B, Propofol, remifentanil and mivacurium: Fast track surgery with poor intubating conditions: Minerva Anestesiol, 2011; 77(6); 7
17. Sayson SC, Mongan PD, Onset of action of mivacurium chloride. A comparison of neuromuscular blockade monitoring at the adductor pollicis and the orbicularis oculi: Anesthesiology, 1994; 81(1); 35-42
18. Plaud B, Debaene B, Donati F, Duration of anesthesia before muscle relaxant injection influences level of paralysis: Anesthesiology, 2002; 97(3); 616-21
19. Hemmerling TM, Schmidt J, Wolf T, Intramuscular versus surface electromyography of the diaphragm for determining neuromuscular blockade: Anesth Analg, 2001; 92(1); 106-11
20. Hemmerling TM, Donati F, Babin D, Beaulieu P, Duration of control stimulation does not affect onset and offset of neuromuscular blockade at the corrugator supercilii muscle measured with phonomyography or acceleromyography: Can J Anesth, 2002; 49(9); 913-17
21. Hemmerling TM, Donati F, Beaulieu P, Babin D, Phonomyography of the corrugator supercilii muscle: signal characteristics, best recording site and comparison with acceleromyography: Br J Anaesth, 2002; 88(3); 389-93
22. Plaud B, Debaene B, Lequeau F, Mivacurium neuromuscular block at the adductor muscles of the larynx and adductor pollicis in humans: Anesthesiology, 1996; 85(1); 77-81
23. Patel N, Kamath N, Smith CE, Intubating conditions and neuromuscular block after divided dose mivacurium or single dose rocuronium: Can J Anaesth, 1997; 44(1); 49-53
24. Honing GHM, Torensma B, Martini CH, Comparison of neuromuscular block measured by compressomyography at the upper arm and electromyography at the adductor pollicis muscle in obese and non-obese patients: An observational study: J Clin Anesth, 2022; 78; 110673
25. Krijtenburg P, Honing G, Martini C: Br J Anaesth, 2019; 122(2); e22-e24
26. Naguib M, Neuromuscular effects of rocuronium bromide and mivacurium chloride administered alone and in combination: Anesthesiology, 1994; 81(2); 388-95
27. Donati F, Bevan DR, Not all muscles are the same: Br J Anaesth, 1992; 68(3); 235-36
28. Plaud B, Baillard C, Bourgain JL, Guidelines on muscle relaxants and reversal in anaesthesia: Anaesth Crit Care Pain Med, 2020; 39(1); 125-42
29. Klein AA, Meek T, Allcock E, Recommendations for standards of monitoring during anaesthesia and recovery 2021: Guideline from the Association of Anaesthetists: Anaesthesia, 2021; 76(9); 1212-23
30. Thilen SR, Hansen BE, Ramaiah R, Intraoperative neuromuscular monitoring site and residual paralysis: Anesthesiology, 2012; 117(5); 964-72
31. Chau I, Horn K, Dullenkopf A: Australas Emerg Care, 2020; 23(4); 217-20
32. Claudius C, Viby-Mogensen J, Warner DS, Warner MA, Acceleromyography for use in scientific and clinical practice – a systematic review of the evidence: Anesthesiology, 2008; 108(6); 1117-40
Figures
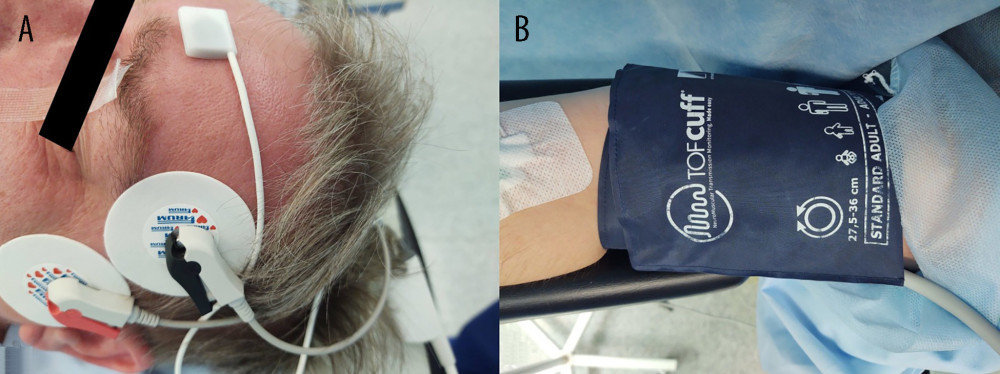 Figure 1. Placement of devices (A) TOF-Scan and (B) TOF-Cuff.
Figure 1. Placement of devices (A) TOF-Scan and (B) TOF-Cuff.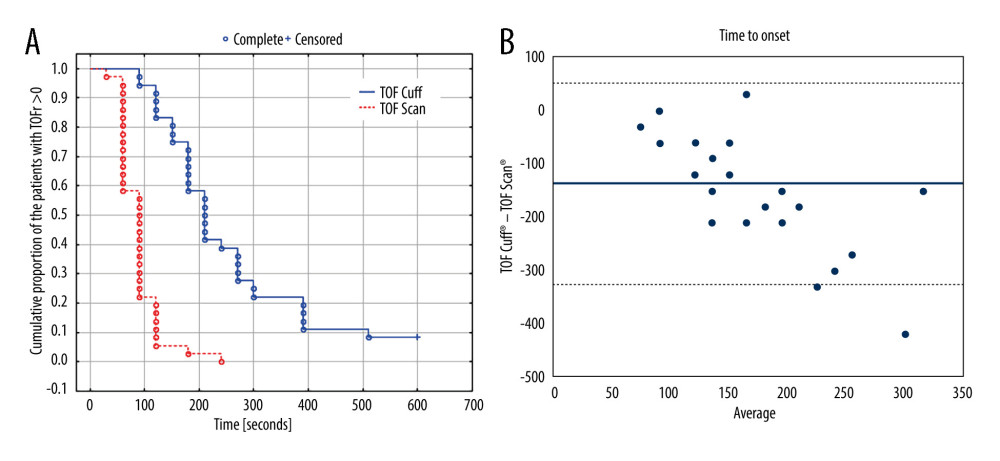 Figure 2. (A) Kaplan-Meier curve presenting time to TOFratio=0 measured with both methods. (Created in: Statistica 13.3, Tibco). (B) The Bland-Altman plot (average vs difference) for onset of neuromuscular block after mivacurium 0.2 mg/kg. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. (Created in: Microsoft Excel 2019). TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle.
Figure 2. (A) Kaplan-Meier curve presenting time to TOFratio=0 measured with both methods. (Created in: Statistica 13.3, Tibco). (B) The Bland-Altman plot (average vs difference) for onset of neuromuscular block after mivacurium 0.2 mg/kg. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. (Created in: Microsoft Excel 2019). TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle.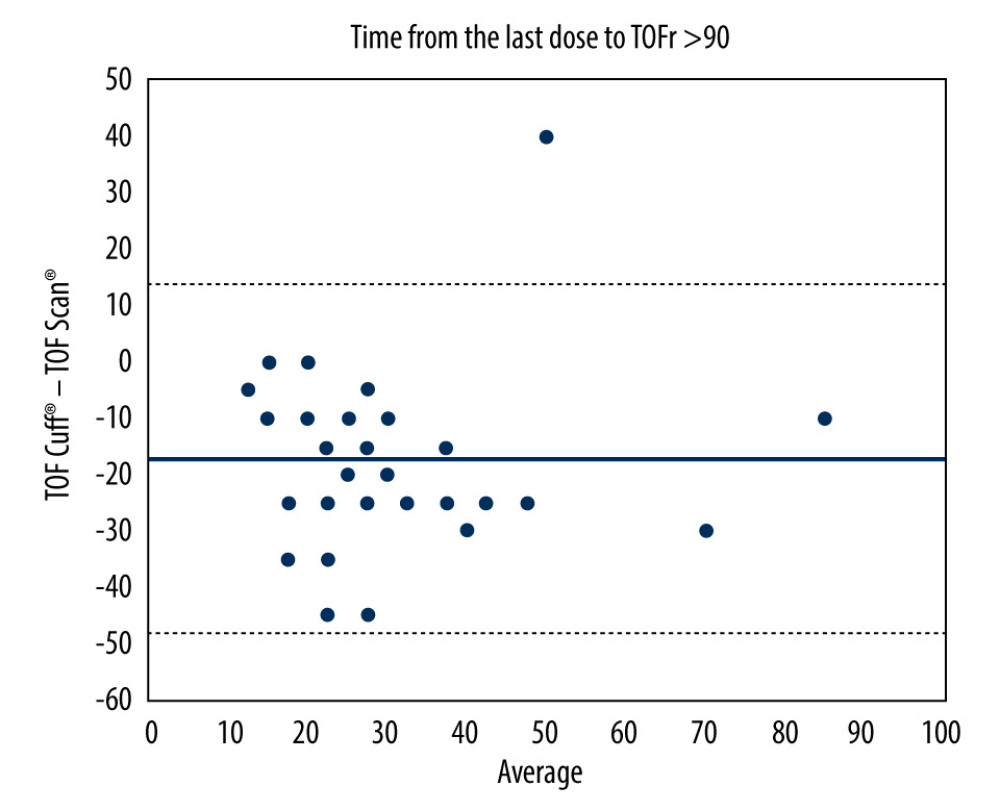 Figure 3. The Bland-Altman plot (average vs difference) for time from the last dose of mivacurium to TOFratio>90. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle. (Created in: Microsoft Excel 2019).
Figure 3. The Bland-Altman plot (average vs difference) for time from the last dose of mivacurium to TOFratio>90. The solid line illustrates the mean difference and the dashed lines indicate average difference ±1.96 standard deviation of the difference. TOF – train-of-four; TOF-Cuff – a device designed for neuromuscular monitoring on an upper arm; TOF-Scan – a device designed for neuromuscular monitoring on a facial corrugator supercilii muscle. (Created in: Microsoft Excel 2019). Tables
 Table 1. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time to TOFratio=0 measured by TOF-Scan against the same time measured by TOF-Cuff.
Table 1. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time to TOFratio=0 measured by TOF-Scan against the same time measured by TOF-Cuff.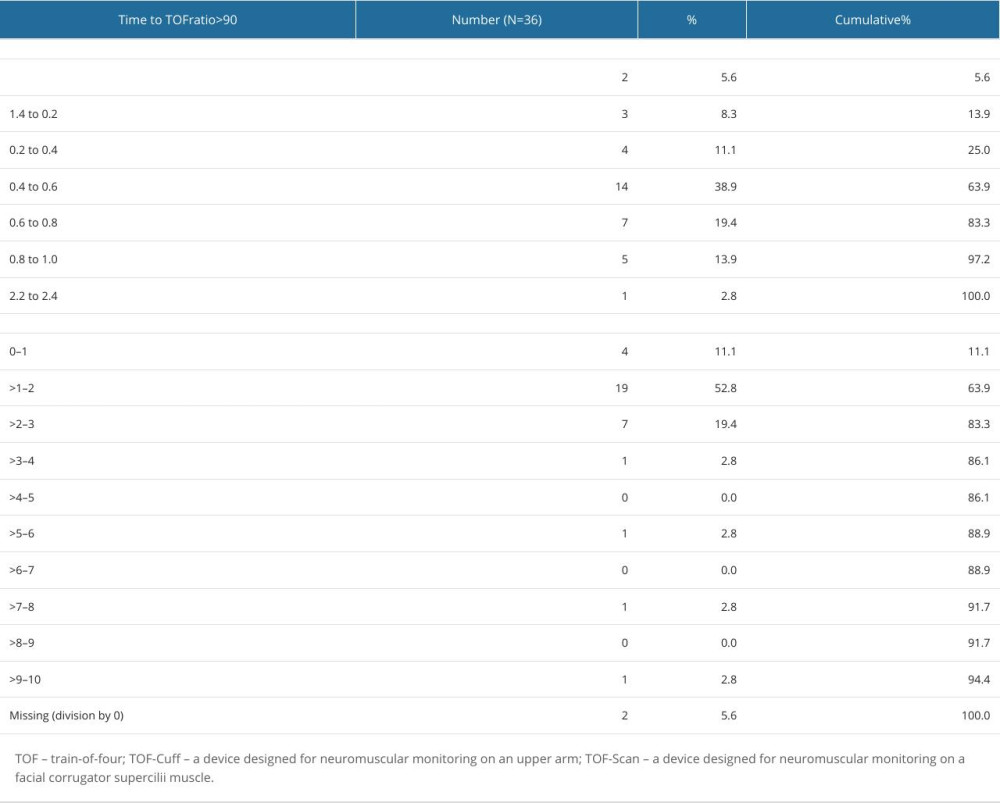 Table 2. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time from the last 2 mg mivacurium dose to TOFratio>90 measured by TOF-Scan against the same time measured by TOF-Cuff.
Table 2. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time from the last 2 mg mivacurium dose to TOFratio>90 measured by TOF-Scan against the same time measured by TOF-Cuff.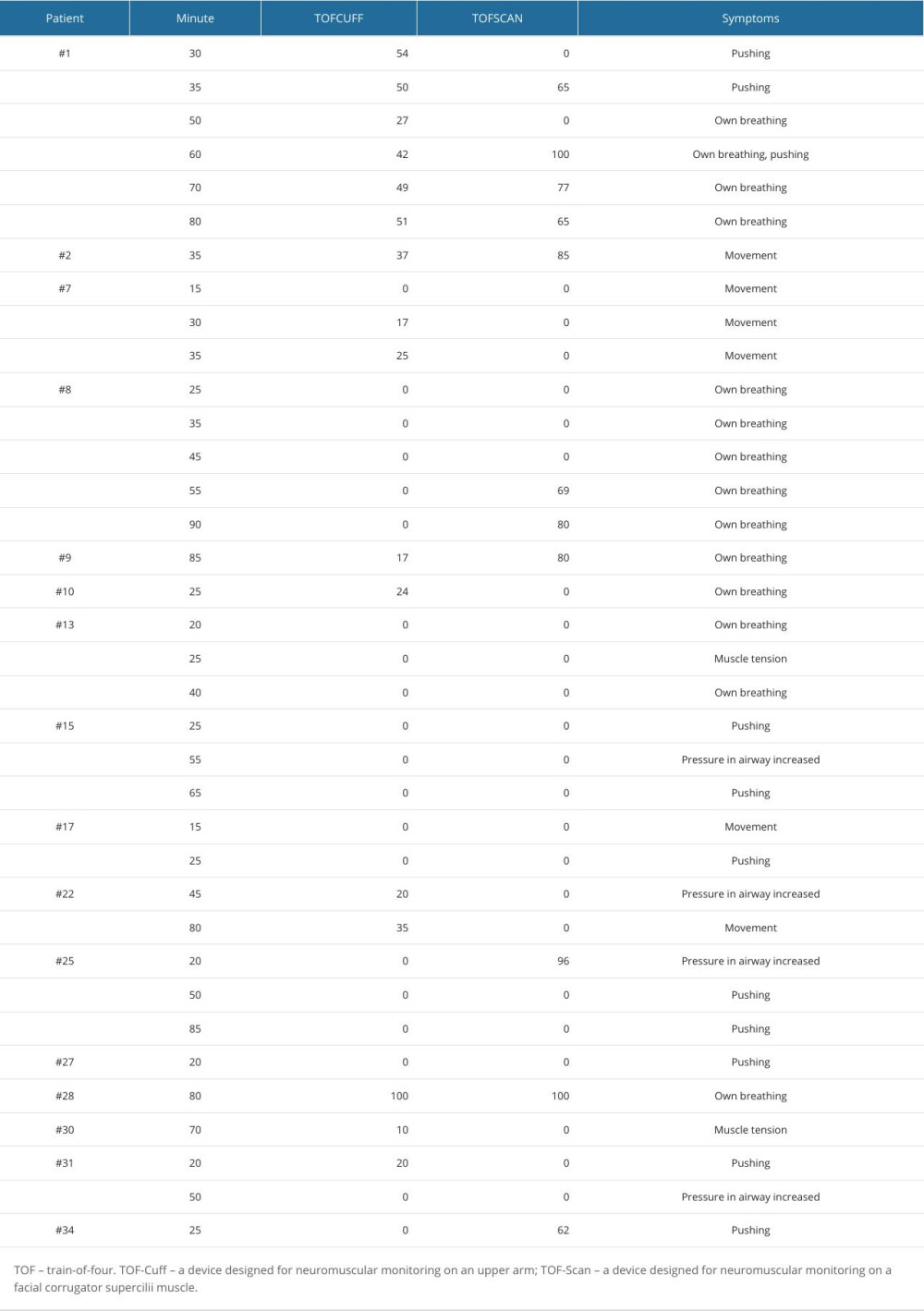 Table 3. Results of TOF (train-of-four) ratio measured with TOF-Cuff and TOF-Scan devices in patients with symptoms resulting in an additional dose of 2 mg mivacurium.
Table 3. Results of TOF (train-of-four) ratio measured with TOF-Cuff and TOF-Scan devices in patients with symptoms resulting in an additional dose of 2 mg mivacurium. Table 1. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time to TOFratio=0 measured by TOF-Scan against the same time measured by TOF-Cuff.
Table 1. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time to TOFratio=0 measured by TOF-Scan against the same time measured by TOF-Cuff.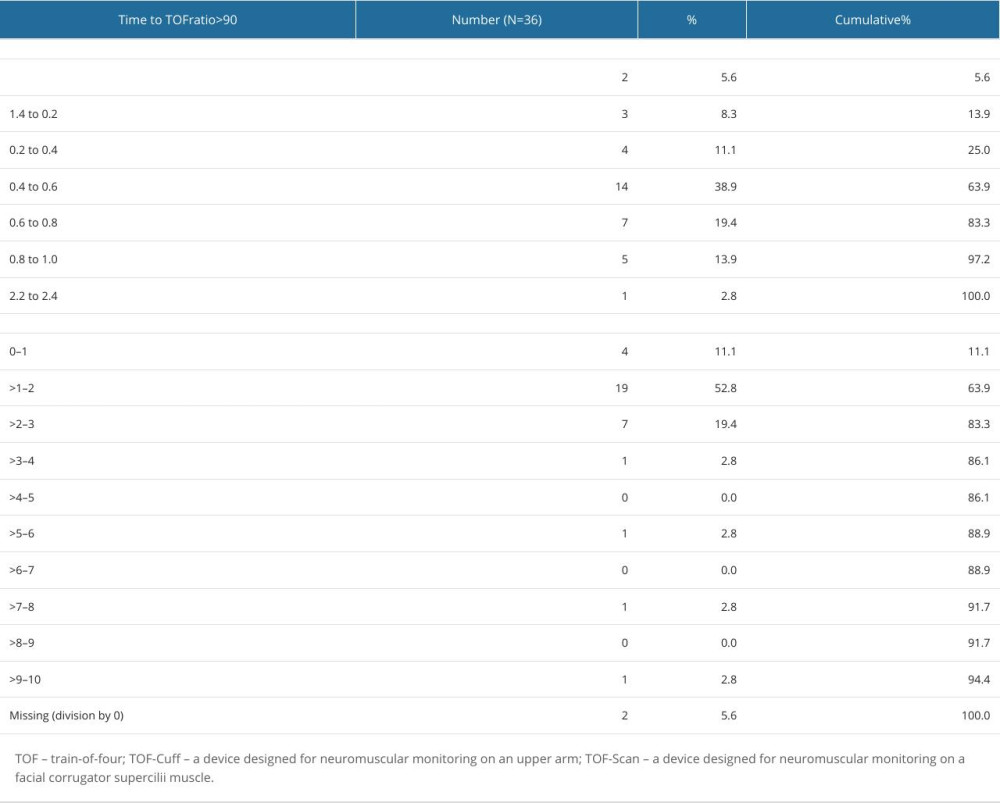 Table 2. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time from the last 2 mg mivacurium dose to TOFratio>90 measured by TOF-Scan against the same time measured by TOF-Cuff.
Table 2. The number, percentage, and cumulative percentage of patients achieving specified ranges of the quotient of time from the last 2 mg mivacurium dose to TOFratio>90 measured by TOF-Scan against the same time measured by TOF-Cuff.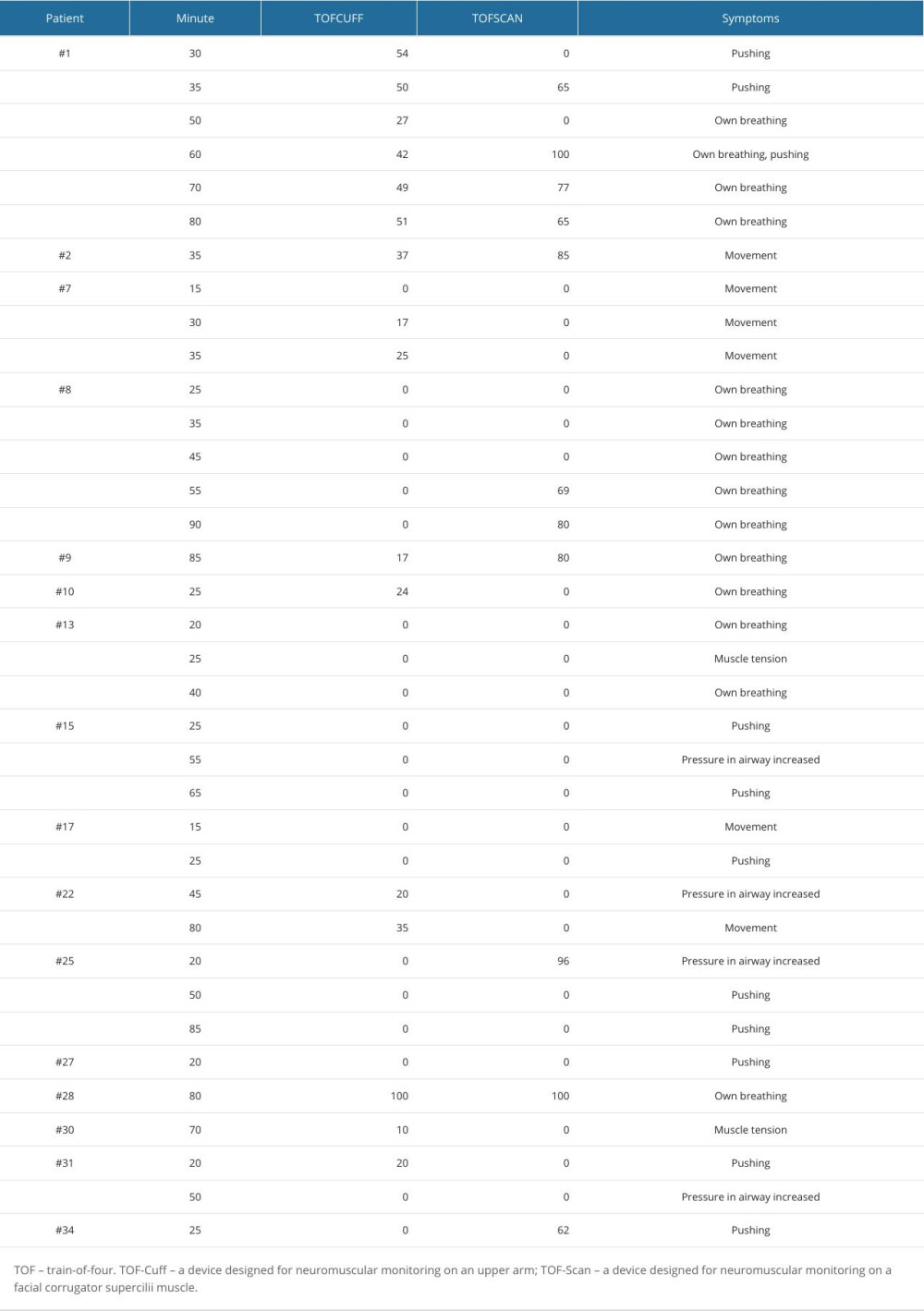 Table 3. Results of TOF (train-of-four) ratio measured with TOF-Cuff and TOF-Scan devices in patients with symptoms resulting in an additional dose of 2 mg mivacurium.
Table 3. Results of TOF (train-of-four) ratio measured with TOF-Cuff and TOF-Scan devices in patients with symptoms resulting in an additional dose of 2 mg mivacurium. In Press
15 Mar 2024 : Clinical Research
Evaluation of an Optimized Workflow for the Radiofrequency Catheter Ablation of Paroxysmal Atrial FibrillationMed Sci Monit In Press; DOI: 10.12659/MSM.943526
09 May 2024 : Review article
A Review of the Current Status of Disease-Modifying Therapies and Prevention of Alzheimer’s DiseaseMed Sci Monit In Press; DOI: 10.12659/MSM.945091
09 Apr 2024 : Clinical Research
Correlation between Thalamocortical Tract and Default Mode Network with Consciousness Levels in Hypoxic-Isc...Med Sci Monit In Press; DOI: 10.12659/MSM.943802
19 Apr 2024 : Clinical Research
Comparative Analysis of Postoperative Sagittal Balance in Expansive Open-Door Laminoplasty versus Laminecto...Med Sci Monit In Press; DOI: 10.12659/MSM.943057
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








