14 April 2024: Clinical Research
Injury-Admission Time is an Independent Risk Factor for Deep Vein Thrombosis in Older Patients with Osteoporotic Hip Fracture
Xiuli Cui1ABCDEF, Qingjun Liu2BCDF, Ronglin Xia1B, Jiaolei Liu2B, Jun Wang1B, Aijun Chao1ABDEF*DOI: 10.12659/MSM.943587
Med Sci Monit 2024; 30:e943587
Abstract
BACKGROUND: Deep vein thrombosis is a common pre- and post-operative complication in older patients with osteoporotic hip fractures. Pre-operative thrombus can increase the risk of surgery. This study examined the association between the time from fracture to admission (injury-admission time) and deep vein thrombosis in older patients with osteoporotic hip fractures.
MATERIAL AND METHODS: Doppler ultrasound screening of deep lower-extremity veins was performed in patients with osteoporotic hip fractures between June 2019 and December 2021. Clinical data, including medical history, injury-admission time, and laboratory tests, were collected retrospectively.
RESULTS: Of the 439 patients, deep vein thrombosis was found in 139 (31.66%). The injury-admission time was significantly longer in the thrombosis group, which was positively associated with deep vein thrombosis (odds ratio 1.010, 95% confidence interval 1.003-1.017). The area under the curve to predict deep vein thrombosis was 0.619. The best cut-off value, sensitivity, and specificity were 21 h, 46.76%, and 75%, respectively. When the injury-admission period exceeded 21 h, the prevalence of deep vein thrombosis was 45.8% and the thrombosis incidence was significantly higher than in the <21 h group (24.9%).
CONCLUSIONS: Our results suggest that screening for deep vein thrombosis should be routinely performed for patients with osteoporotic hip fractures, particularly for those with injury-admission time ≥21 h.
Keywords: Osteoporotic Fractures, Risk Factors, Venous Thrombosis
Introduction
Osteoporotic fractures are more likely to occur in older people, among which hip fracture is common [1]. Deep vein thromboses (DVT) commonly follow hip fractures in older adults, which affects fracture treatment and functional recovery, and can even be fatal [2]. Patients with hip fractures are at risk of developing DVT in both the preoperative and postoperative periods. A meta-analysis suggested that the risk factors of preoperative DVT for hip fracture included female patients, advanced age, coronary heart disease, prolonged time from injury to surgery, and C-reactive protein [3]. Data from previous studies show that the preoperative incidence of DVT after hip fracture is 2.6% [4]. Another study found that approximately 30% of patients with hip fractures develop DVT before surgery [5]. In addition, 20.1% of older patients with intertrochanteric fractures had DVT at admission, with approximately 30% of them having proximal thrombosis [6]. These data illustrate that some patients with fracture already had DVT prior to surgery. In older patients with hip fracture, the incidence of DVT increases if the time from injury to surgery exceeds 48 h. Therefore, a surgical delay of more than 48 h is a risk factor for VTE [7]. The guidelines recommend surgery in older patients with hip fractures within 24–48 h [8]. If DVT is already present at admission, surgery increases the risk of thrombus shedding. Traumatic stress and hypercoagulability peak at 1–4 days after trauma [9], with an increased risk of thrombosis. Therefore, injury-admission time affects DVT occurrence. However, limited data are available regarding the incidence of DVT at hospital admission. The primary aim of this study was to examine the association between injury-admission time and DVT in older patients with osteoporotic hip fractures.
Material and Methods
STUDY DESIGN:
Data from patients with osteoporotic hip fractures (≥65 years old) who were hospitalized between June 2019 and December 2021 were retrospectively collected. Venous Doppler ultrasonography was performed on both lower limbs on admission. Based on examination of the total femoral vein, the superficial femoral, deep femoral, popliteal, tibial, and sural veins were examined sequentially. The Medical Ethics Committee of the Tianjin Hospital approved this study (ethics approval number: 2023YLS044). A waiver for informed consent was obtained for this study owing to its retrospective nature.
INCLUSION AND EXCLUSION CRITERIA:
The inclusion criteria were closed hip fracture (including intertrochanteric, femoral neck, and subtrochanteric fractures) that occurred within 7 days after the trauma, which required hospitalization and an osteoporosis diagnosis. Osteoporotic fracture is a fracture occurring due to decreased bone strength or increased bone fragility due to low-energy external forces or daily activities [10].
The exclusion criteria were pathological or open fracture, injury for more than 7 days, multiple fractures, multiple injuries, anticoagulation therapy before the injury, history of thrombosis, severe kidney and liver dysfunction, malignant tumors, blood system diseases, acute cardiovascular and cerebrovascular diseases, abnormal muscle strength of the lower limbs before injury, non-osteoporotic fractures, and incomplete clinical data.
CLINICAL DATA COLLECTION:
Relevant clinical data of patients who fulfilled the enrollment criteria were retrospectively collected, which included sex, age, body mass index (BMI), medical history (chronic obstructive pulmonary disease, type 2 diabetes mellitus, high blood pressure, coronary heart disease [CHD], cerebral infarction, cerebral hemorrhage, and fracture), injury-admission time (the time from fracture to admission), and laboratory test results (levels of white blood cells, middle granulocytes, platelets, monocytes, lymphocytes, high-density lipoprotein, C-reactive protein, superoxide dismutase, and D-dimer).
STATISTICAL ANALYSIS:
SPSS software, version 26.0 (SPSS for Windows, IBM Corp., Armonk, NY, USA), and MedCalc statistical software 19 (MedCalc Software, Ostend, Belgium) were used for statistical analyses. Continuous variables are expressed as mean±standard deviation (SD), and the normality of the data was examined. Data that did not meet the normal distribution requirement are expressed as medians (Q1, Q3). If the data were normally distributed, the
Results
PATIENT CHARACTERISTICS:
In this study, 439 individuals were included. This group comprised 114 males (26.0%) and 325 females (74.0%). No significant difference in age was observed between sexes (male: 80.4 years, female: 81.76 years; z=−0.815;
COMPARISON OF COUNT DATA BETWEEN THE THROMBOSIS AND NON-THROMBOSIS GROUPS:
The proportion of patients with CHD and history of cerebral infarction was significantly lower in the thrombosis group than in the non-thrombosis group (Table 1).
COMPARISON OF PHYSIOLOGICAL AND LABORATORY MEASURES BETWEEN THE THROMBOSIS AND NON-THROMBOSIS GROUPS:
BMI, injury-admission time, lymphocytes (LYM), neutrophil-lymphocyte ratio (NLR), monocyte to high-density lipoprotein ratio (MHR), C-reactive protein (CRP), superoxide dismutase (SOD), and D-dimer levels were significantly different between the thrombosis and non-thrombosis groups. The median distributions of BMI, injury-admission time, LYM, MHR, and CRP in the thrombosis group were higher than that in the non-thrombosis group, and the median distributions of NLR, SOD, and D-dimer were lower in the thrombosis group than in the non-thrombosis group (Table 2).
MULTIVARIATE LOGISTIC REGRESSION ANALYSIS OF RISK-RELATED FACTORS FOR DVT:
Taking the occurrence of thrombosis as the dependent variable, the variables with P<0.5 were analyzed by logistic regression. The results showed that the factors related to thrombosis occurrence were CHD, history of cerebral infarction, injury-admission time, SOD levels, and D-dimer levels. Risk factors included injury-admission time (odds ratio [OR], 1.010; 95% confidence interval [CI] 1.003–1.017). Protective factors included CHD (OR, 0.564; 95% CI 0.360–0.883), history of cerebral infarction (OR, 0.021; 95% CI 0.334–0.913), SOD levels (OR, 0.989; 95% CI 0.980–0.999), and D-dimer levels (OR, 0.9998; 95% CI 0.9996–0.9999; Table 3; Figure 1).
PREDICTIVE VALUE OF INJURY-ADMISSION TIME ON DVT INCIDENCE:
The area under the curve (AUC) of injury-admission time to predict DVT was 0.619 (95% CI 0.572–0.665; P=0.0001). A cut-off value of 21 h was chosen. The sensitivity and specificity were 46.76% and 75%, respectively (Figure 2). Data were grouped according to the 21 h cut-off value, and the occurrence of thrombosis was compared between the 2 groups. In the ≥21 h group, the thrombosis rate was 45.8%, which was a significantly higher than the 24.9% observed in the <21 h group (Table 4).
Discussion
Older adults are more likely to develop DVT after a hip fracture, increasing the length and cost of their hospital stays [2]. In this study, 139 patients (31.66%) with osteoporotic hip fractures were found to have DVT upon admission, including 79 (56.83%) with intermuscular venous thrombosis and 60 (43.17%) with non-intermuscular venous thrombosis. A previous study indicated that the proportion of DVT that occurred in aged populations with osteoporotic hip fracture before the operation was 29.4% [5]. Another study revealed that DVT was detected in 29.8% of older patients diagnosed with hip fractures [11], reaffirming the level of DVT occurrence found in our study. Consequently, older people with osteoporotic hip fractures have a higher risk of developing DVT.
In the thrombosis group, we observed a significantly lower proportion of patients with CHD and a history of cerebral infarction than in the non-thrombosis group. Multivariate regression analysis indicated that these factors were protective. Moreover, 28.5% (72/253) of the patients with CHD and a history of cerebral infarction took antiplatelet drugs. Aspirin is the most-used antiplatelet drug; it can decrease thromboxane A2 production in platelets, reduce the number of NF-κB-positive cells and the expression of NF-κB protein, and reduce local inflammatory responses [12]. Another study found that aspirin reduced the risk of venous thromboembolism (VTE) recurrence by 44% [13]. Moreover, studies have shown that aspirin can prevent the occurrence of VTE after hip arthroplasty [14]. Although no significant difference in the use of antiplatelet drugs was observed between the 2 groups in our study, 20% of patients in the non-thrombosis group received antiplatelet treatment, which was higher than in the thrombosis group. Therefore, we speculate that the decreased VTE risk in patients with hip fractures may be associated with the use of antiplatelet drugs.
In this study, the median values of BMI, injury-admission time, LYM, MHR, and CRP in the thrombosis group were significantly higher than those in the non-thrombosis group, whereas the median values of NLR, SOD, and D-dimer were lower in the thrombosis group than the median values in the non-thrombosis group, as assessed by univariate analysis. Regression analysis of these variables revealed that the occurrence of DVT was associated with SOD, D-dimer level, and injury-admission time. SOD and D-dimer were negatively correlated with DVT, and prehospital time was positively correlated with DVT.
Oxidative stress occurring after a fracture plays a significant role in regulating platelet and leukocyte activation, mediating the mutual adhesion between venous endothelial cells, platelets, and leukocytes, promoting thrombus formation [15]. Moreover, the generation of a large amount of reactive oxygen species is the key to thrombosis [16]. In the thrombosis group in this study, large quantities of SOD, which exhibits antioxidant properties, were consumed, resulting in decreased SOD levels. SOD was also negatively correlated with the occurrence of DVT and was a protective factor against DVT in aged adults with osteoporotic hip fractures.
Fractures are often accompanied by an increase in D-dimer levels. Therefore, some studies indicated that normal D-dimer levels cannot exclude thrombus in patients with trauma [17]. The thrombosis group had lower D-dimer levels than the non-thrombosis group in this study. There are data revealing that D-dimer peaks within 48 h in patients with trauma. It is not suitable to judge the occurrence of thrombosis within 48 h [18]. We hypothesize that the reason may be that D-dimer has a half-life of 7–8 h and D-dimer levels are influenced by the balance of the blood coagulation and fibrinolytic systems in the body [19]. In the thrombus group, the injury-admission time was 14±42 h, which was significantly longer than the half-life of D-dimer. This may be the underlying cause for the low D-dimer levels.
Different fracture sites lead to different proportions of DVT, and the incidence of DVT is the highest for limb trauma. Most of the DVT cases occurred within 7 days after the fracture [20], which may be related to the hypercoagulable state following fractures. Researchers have analyzed the perioperative period of fracture and found that the preoperative time of patients with DVT was significantly longer, which is a risk factor for DVT [21]. Various studies have consistently demonstrated that older patients with a prolonged preoperative time after hip fractures are more likely to experience DVT [22,23]. With a longer interval from injury to surgery, the incidence of DVT gradually rose to 36.2% in patients waiting for more than 7 days [24]. In a nomogram model predicting the risk of preoperative DVT in older adults with hip fracture, injury-admission time was one of the main risk factors and accounted for a large weight. In the thrombotic group, the injury-admission time was 3.08±1.37 days, which was significantly longer than in the non-thrombotic group [25]. In the present study, the injury-admission time in the thrombus group was 14±42 h, which was shorter than that observed in previous studies. Prolonging the injury-admission time after a hip fracture increased the risk of thrombosis, and injury-admission time was identified as an independent factor for developing DVT in older patients with osteoporotic hip fractures. The AUC in our study was 0.619, and the cut-off value was 21 h when the injury-admission time was used to predict the occurrence of DVT. When the injury-admission time was ≥21 h, the incidence of thrombosis was 45.8%, which demonstrated that the incidence of thrombosis was close to 50%. Based on this finding, we suggest that older patients with osteoporotic hip fractures should routinely undergo Doppler ultrasound of the lower limbs, particularly patients with an injury-admission time ≥21 h, and need anticoagulation treatment as soon as possible if there is no contraindication. The cut-off time recommended here is earlier than previously specified. This difference might be related to the following 2 reasons. First, the study parameter was the time from injury to admission. Second, the injury-admission time of the included patients was shorter than those in the above studies from the literature. Guidelines suggest a better prognosis for surgery within 48 h of admission [26]. DVT increases the risk of surgery and should be evaluated at the earliest possible time. Therefore, in the present study, the cut-off time of DVT has more clinical value.
This study had some limitations. First, it was a retrospective study, which might inevitably ignore certain influencing factors. Second, although we included all eligible patients during the study period, the sample size was still limited. In future, we plan to conduct prospective studies to further investigate the risk of thrombosis in older patients with hip fractures.
Conclusions
In older patients with osteoporotic hip fractures, significantly longer injury-admission time is an independent risk factor for DVT. The incidence of DVT in this specific patient population was 31.66%. In our study, the risk of DVT significantly increased when the injury-admission time exceeded 21 h. Older patients with osteoporotic hip fractures should be carefully monitored for DVT symptoms, particularly for those with injury-admission ≥21 h.
Figures
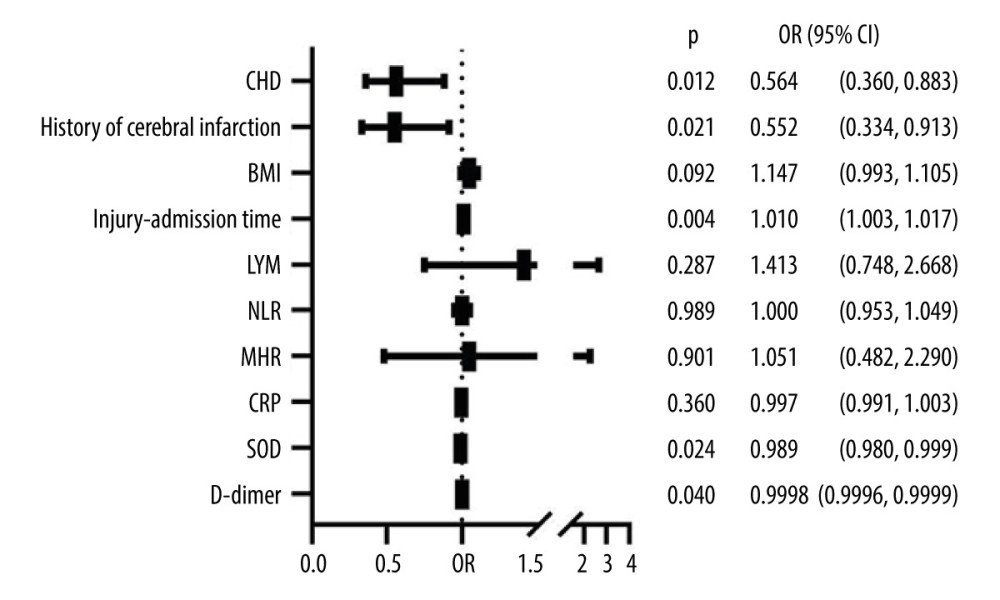 Figure 1. Multivariate logistic regression analysis of DVT risk. BMI – body mass index; CI – confidence interval; CRP – C-reactive protein; DVT – deep vein thrombosis; MHR – monocyte to high-density lipoprotein ratio; NLR – neutrophil-lymphocyte ratio; OR – odds ratio; SOD – superoxide dismutase. Created using GraphPad Prism version 9.5.1 (GraphPad Software).
Figure 1. Multivariate logistic regression analysis of DVT risk. BMI – body mass index; CI – confidence interval; CRP – C-reactive protein; DVT – deep vein thrombosis; MHR – monocyte to high-density lipoprotein ratio; NLR – neutrophil-lymphocyte ratio; OR – odds ratio; SOD – superoxide dismutase. Created using GraphPad Prism version 9.5.1 (GraphPad Software). 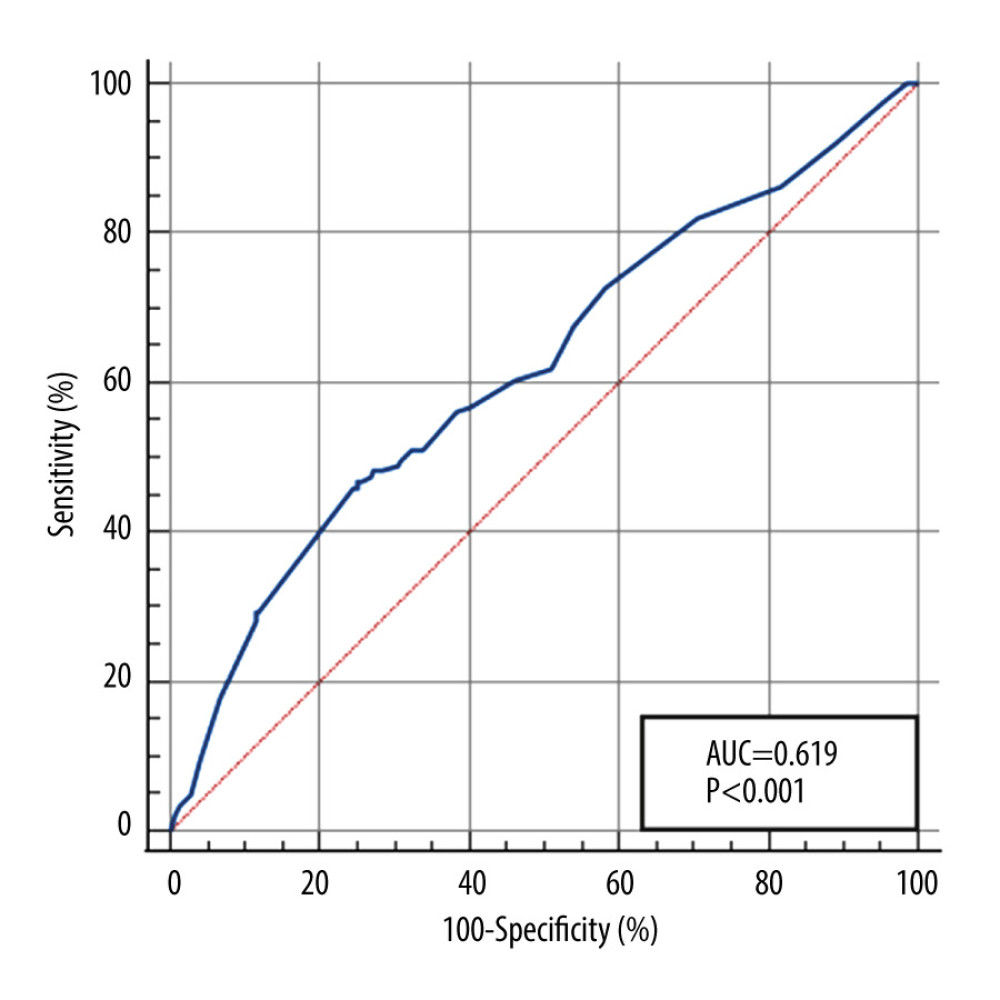 Figure 2. The predictive value of injury-admission time for deep vein thrombosis. Created using MedCalc version19 (MedCalc Software).
Figure 2. The predictive value of injury-admission time for deep vein thrombosis. Created using MedCalc version19 (MedCalc Software). References
1. Veronese N, Maggi S, Epidemiology and social costs of hip fracture: Injury, 2018; 49; 1458-60
2. Shin WC, Lee SM, Suh KT, Recent updates of the diagnosis and prevention of venous thromboembolism in patients with a hip fracture: Hip Pelvis, 2017; 29; 159-67
3. Wang T, Guo J, Long Y, Risk factors for preoperative deep venous thrombosis in hip fracture patients: A meta-analysis: J Orthop Traumatol, 2022; 23; 19
4. Cho YH, Byun YS, Jeong DG, Preoperative incidence of deep vein thrombosis after hip fractures in Korean: Clin Orthop Surg, 2015; 7; 298-302
5. Song K, Yao Y, Rong Z, The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures: Arch Orthop Trauma Surg, 2016; 136; 1459-64
6. Zuo J, Hu Y, Admission deep venous thrombosis of lower extremity after intertrochanteric fracture in the elderly: A retrospective cohort study: J Orthop Surg Res, 2020; 15; 549
7. Taoka T, Ohmori T, Kanazawa T, Delayed surgery after hip fracture affects the incidence of venous thromboembolism: J Orthop Surg Res, 2023; 18; 630
8. O’Connor MI, Switzer JA, AAOS Clinical Practice Guideline Summary: Management of hip fractures in older adults: J Am Acad Orthop Surg, 2022; 30; e1291-96
9. Schreiber MA, Differding J, Thorborg P, Hypercoagulability is most prevalent early after injury and in female patients: J Trauma, 2005; 58; 475-81
10. Chinese Orthopaedic Association, Guidelines for the diagnosis and treatment of osteoporotic fractures (2022 edition): Chin J Orthop, 2022; 42; 1473-91
11. Xing F, Li L, Long Y, Admission prevalence of deep vein thrombosis in elderly Chinese patients with hip fracture and a new predictor based on risk factors for thrombosis screening: BMC Musculoskelet Disord, 2018; 19; 444
12. Wang LC, Jiang RL, Zhang W, Effects of aspirin on the expression of nuclear factor-κB in a rat model of acute pulmonary embolism: World J Emerg Med, 2014; 5; 229-33
13. Rabinowitz I, Aspirin reduced recurrence of venous thromboembolism (VTE) after a first-ever, unprovoked VTE: Ann Intern Med, 2012; 157; JC4-3
14. Chisari E, Tan TL, Shah R, Aspirin is an effective prophylaxis for venous thromboembolism in ambulatory patients with femoral neck fracture undergoing hip arthroplasty: J Bone Joint Surg Am, 2022; 104; 603-9
15. Chakrabarti S, Rizvi M, Pathak D, Hypoxia influences CD40-CD40L mediated inflammation in endothelial and monocytic cells: Immunol Lett, 2009; 122; 170-84
16. Re G, Lanzarini C, Vaona I, Systemically circulating oxidative species in human deep venous thrombosis: Eur J Emerg Med, 1998; 5; 9-12
17. Wahl WL, Ahrns KS, Zajkowski PJ, Normal D-dimer levels do not exclude thrombotic complications in trauma patients: Surgery, 2003; 134; 529-32
18. Owings JT, Gosselin RC, Anderson JT, Practical utility of the D-dimer assay for excluding thromboembolism in severely injured trauma patients: J Trauma Acute Care Surg, 2001; 51; 425-30
19. Favresse J, Lippi G, Roy PM, D-dimer: Preanalytical, analytical, postanalytical variables, and clinical applications: Crit Rev Clin Lab Sci, 2018; 55; 548-77
20. Zhu Y, Chen W, Li J, Incidence and locations of preoperative deep venous thrombosis (DVT) of lower extremity following tibial plateau fractures: A prospective cohort study: J Orthop Surg Res, 2021; 16; 113
21. Zhang W, Huai Y, Wang W, A Retrospective cohort study on the risk factors of deep vein thrombosis (DVT) for patients with traumatic fracture at Honghui Hospital: BMJ Open, 2019; 9; e024247
22. Rodriguez-Fernandez P, Adarraga-Cansino D, Carpintero P, Effects of delayed hip fracture surgery on mortality and morbidity in elderly patients: Clin Orthop Relat Res, 2011; 469; 3218-21
23. Bengoa F, Vicencio G, Schweitzer D, High prevalence of deep vein thrombosis in elderly hip fracture patients with delayed hospital admission: Eur J Trauma Emerg Surg, 2020; 46; 913-17
24. Cong Y, Huang H, Zhang BF, The correlation between preoperative lower extremity deep vein thrombosis (DVT) and the time from injury to surgery (TFITS): Clin Appl Thromb Hemost, 2022; 28; 10760296221108961
25. Zhang L, He M, Jia W, Analysis of high-risk factors for preoperative DVT in elderly patients with simple hip fractures and construction of a nomogram prediction model: BMC Musculoskelet Disord, 2022; 23; 441
26. Brox WT, Roberts KC, Taksali S, The American Academy of Orthopaedic Surgeons evidence-based guideline on management of hip fractures in the elderly: J Bone Joint Surg Am, 2015; 97; 1196-99
Figures
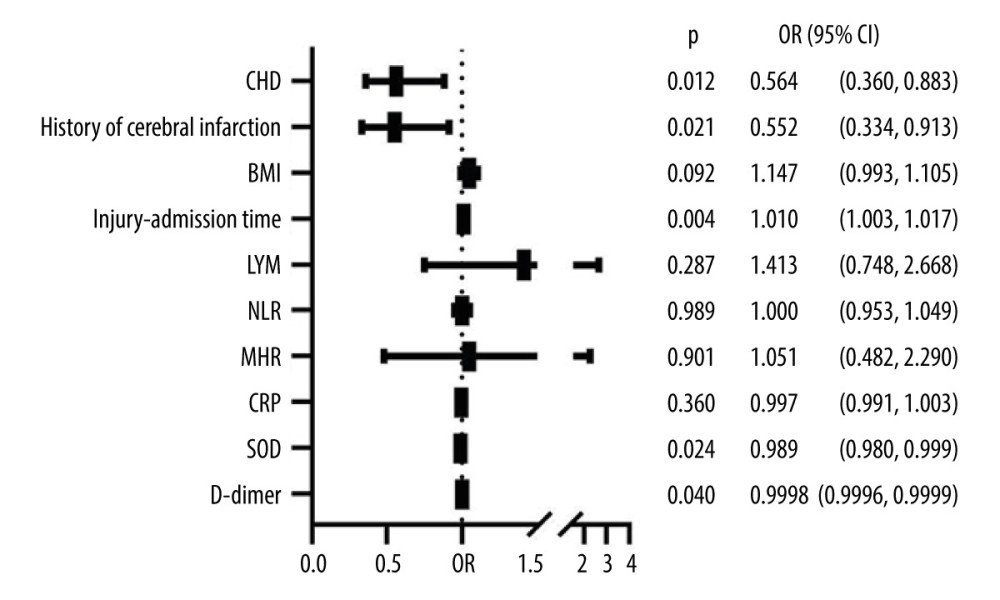 Figure 1. Multivariate logistic regression analysis of DVT risk. BMI – body mass index; CI – confidence interval; CRP – C-reactive protein; DVT – deep vein thrombosis; MHR – monocyte to high-density lipoprotein ratio; NLR – neutrophil-lymphocyte ratio; OR – odds ratio; SOD – superoxide dismutase. Created using GraphPad Prism version 9.5.1 (GraphPad Software).
Figure 1. Multivariate logistic regression analysis of DVT risk. BMI – body mass index; CI – confidence interval; CRP – C-reactive protein; DVT – deep vein thrombosis; MHR – monocyte to high-density lipoprotein ratio; NLR – neutrophil-lymphocyte ratio; OR – odds ratio; SOD – superoxide dismutase. Created using GraphPad Prism version 9.5.1 (GraphPad Software).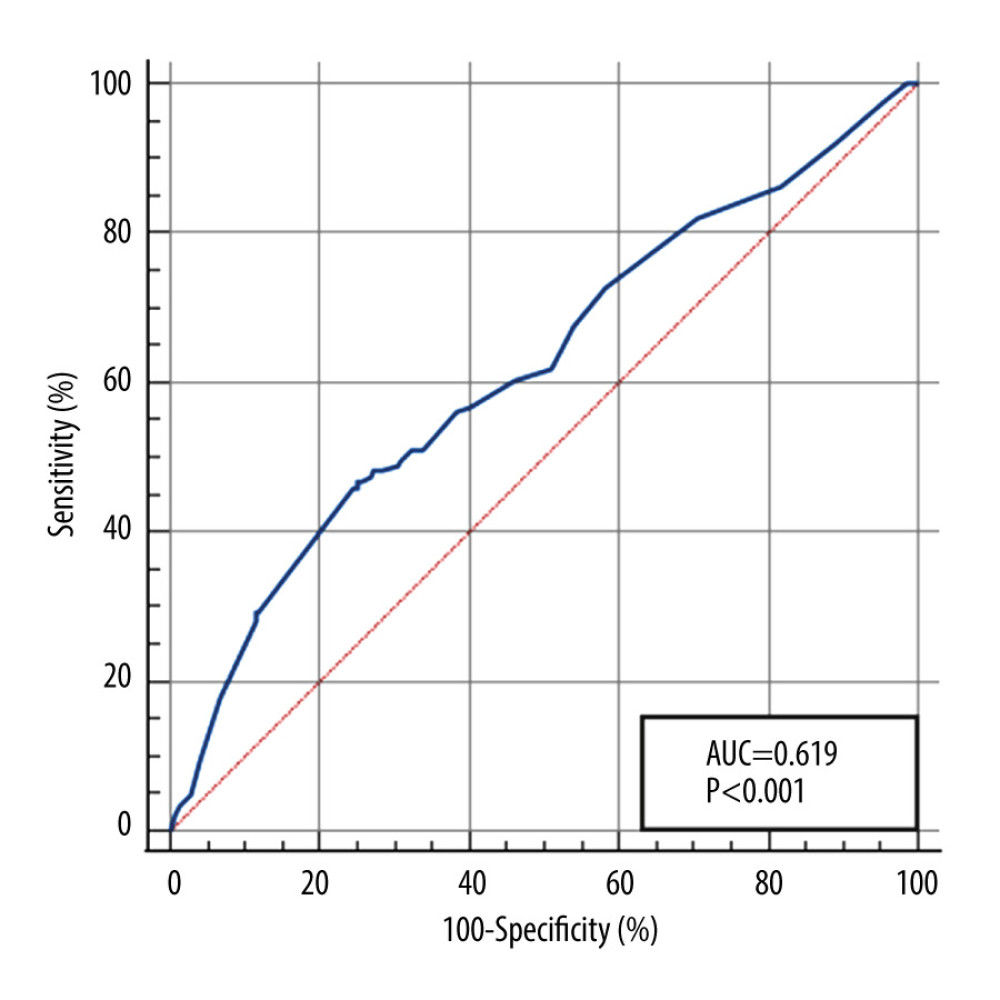 Figure 2. The predictive value of injury-admission time for deep vein thrombosis. Created using MedCalc version19 (MedCalc Software).
Figure 2. The predictive value of injury-admission time for deep vein thrombosis. Created using MedCalc version19 (MedCalc Software). Tables
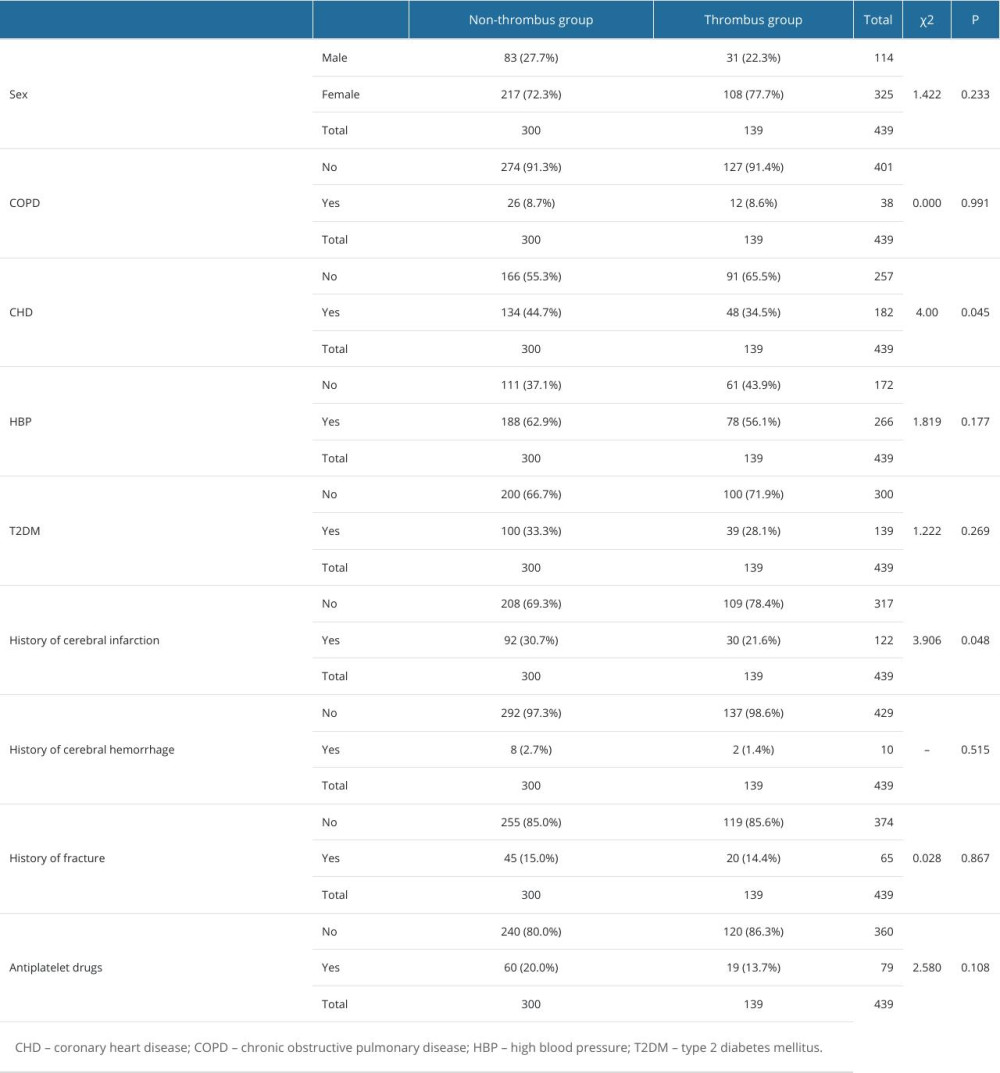 Table 1. Comparison of count data between groups.
Table 1. Comparison of count data between groups.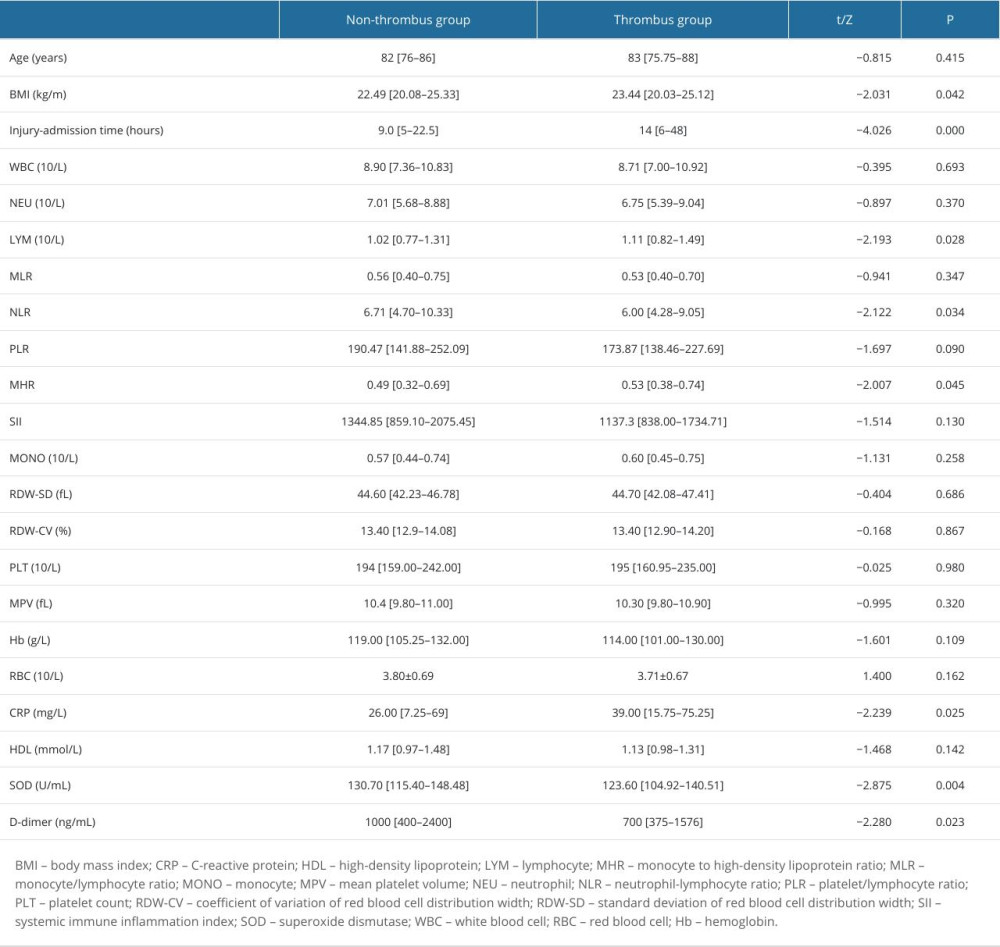 Table 2. Comparison of selected measurement parameters between the 2 groups.
Table 2. Comparison of selected measurement parameters between the 2 groups.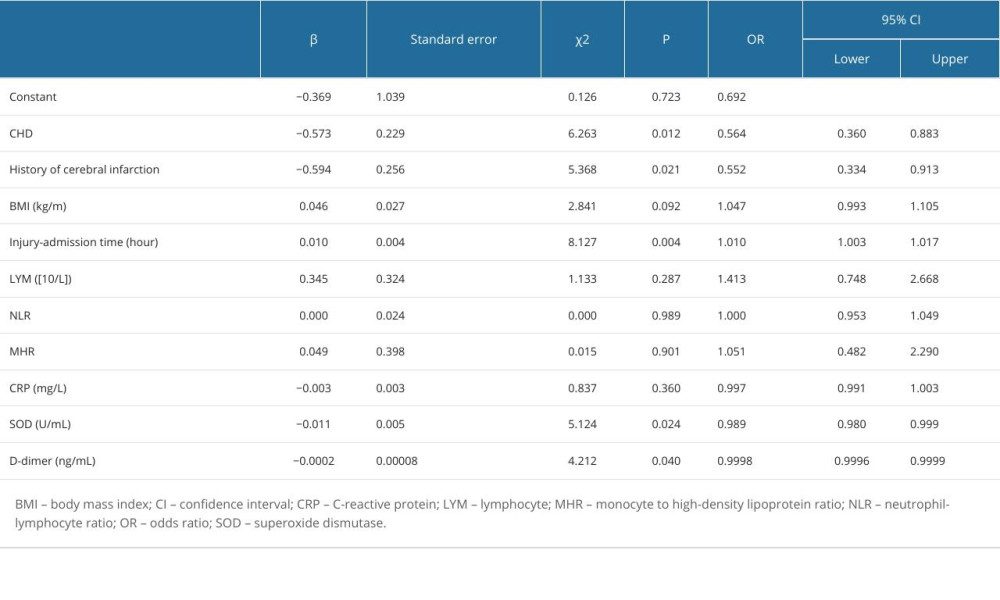 Table 3. Multivariate logistic regression analysis of DVT risk.
Table 3. Multivariate logistic regression analysis of DVT risk.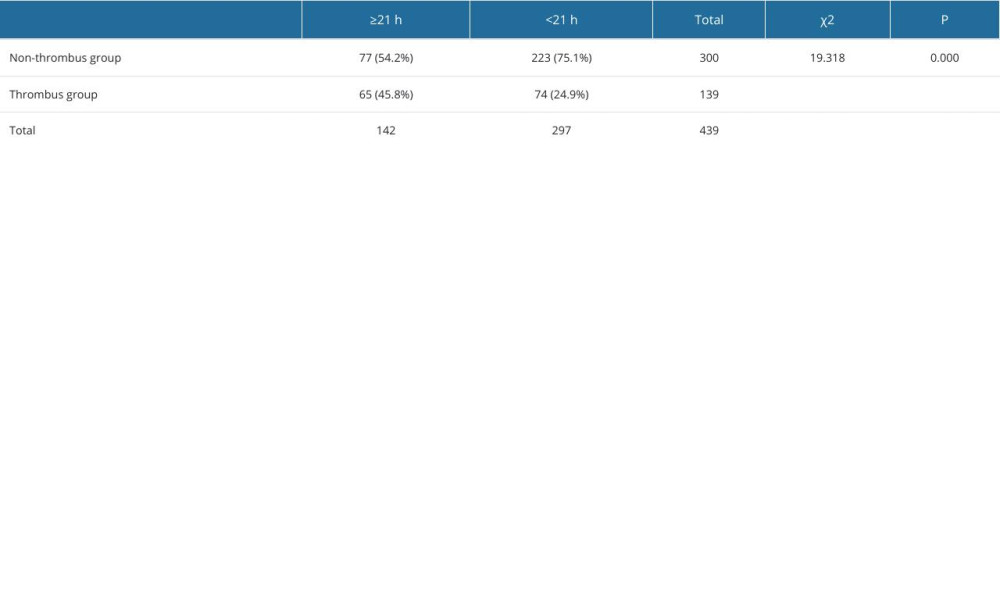 Table 4. Occurrence of thrombus according to the best cut-off value.
Table 4. Occurrence of thrombus according to the best cut-off value.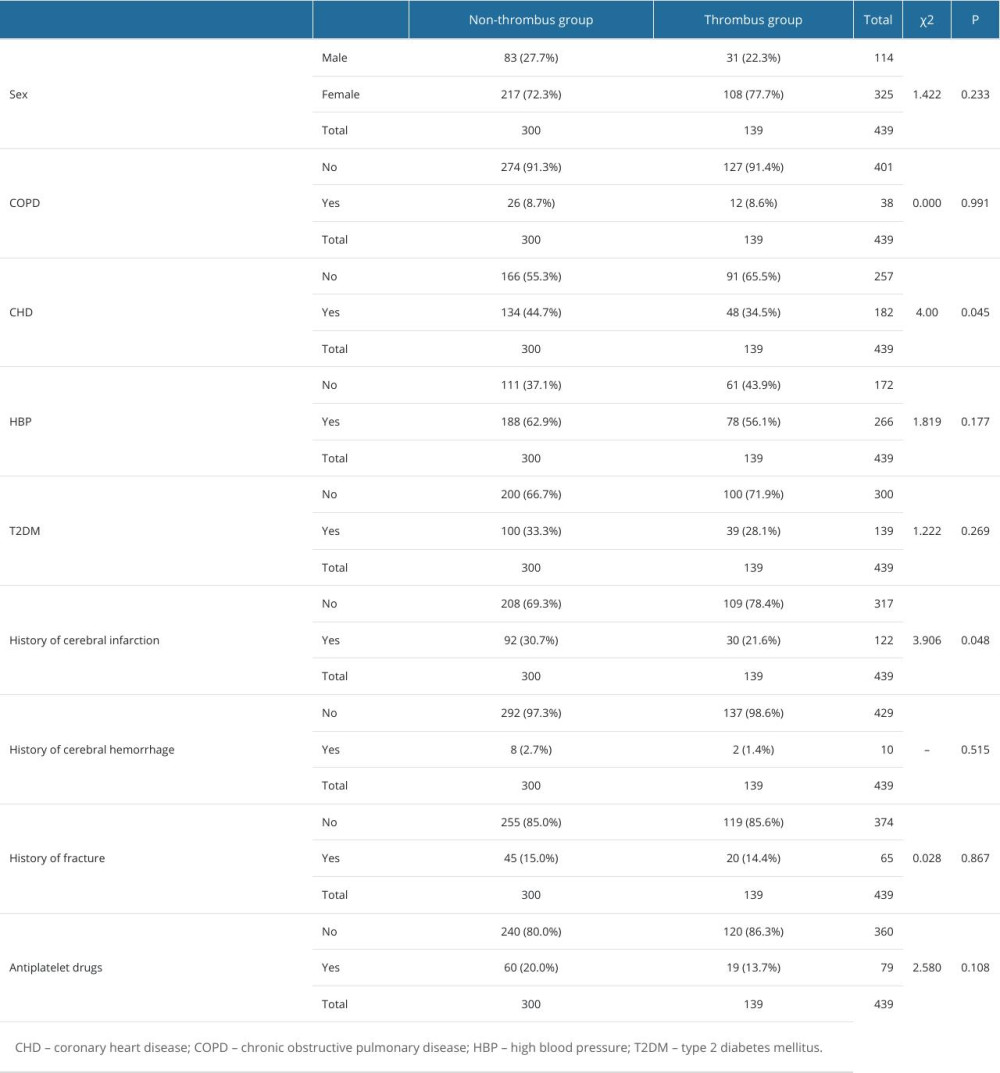 Table 1. Comparison of count data between groups.
Table 1. Comparison of count data between groups.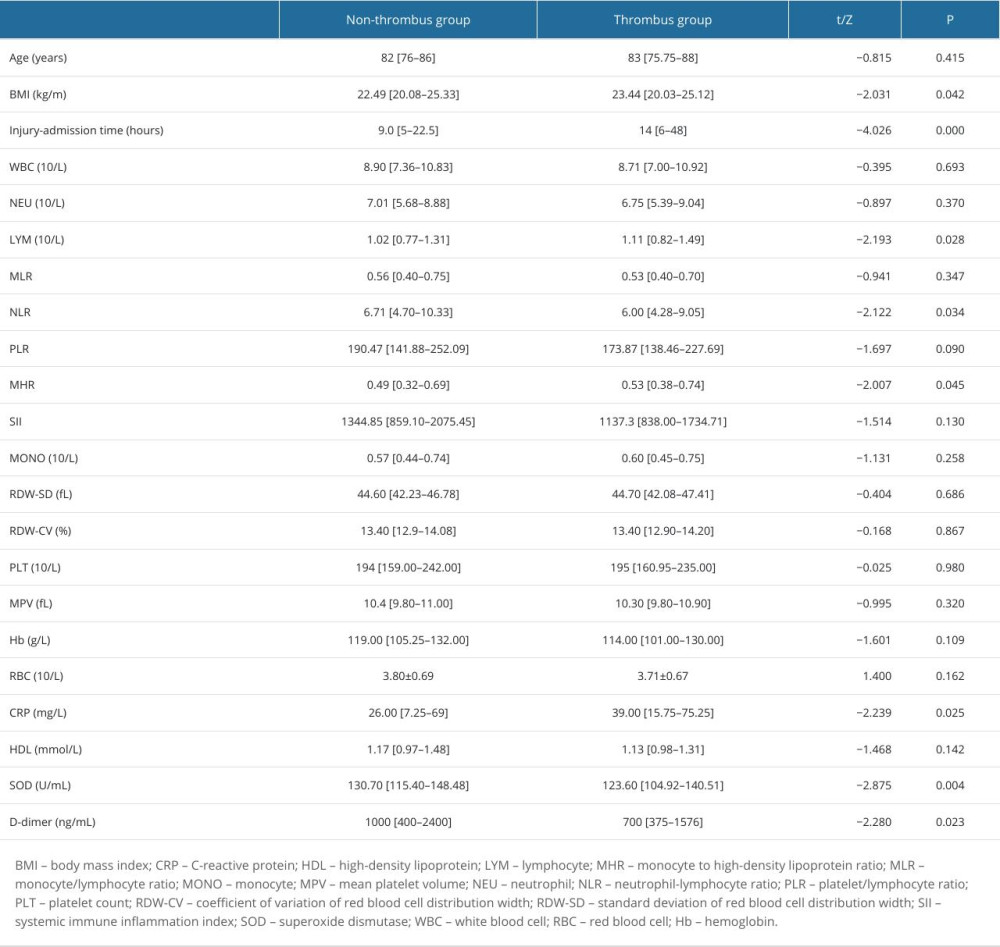 Table 2. Comparison of selected measurement parameters between the 2 groups.
Table 2. Comparison of selected measurement parameters between the 2 groups.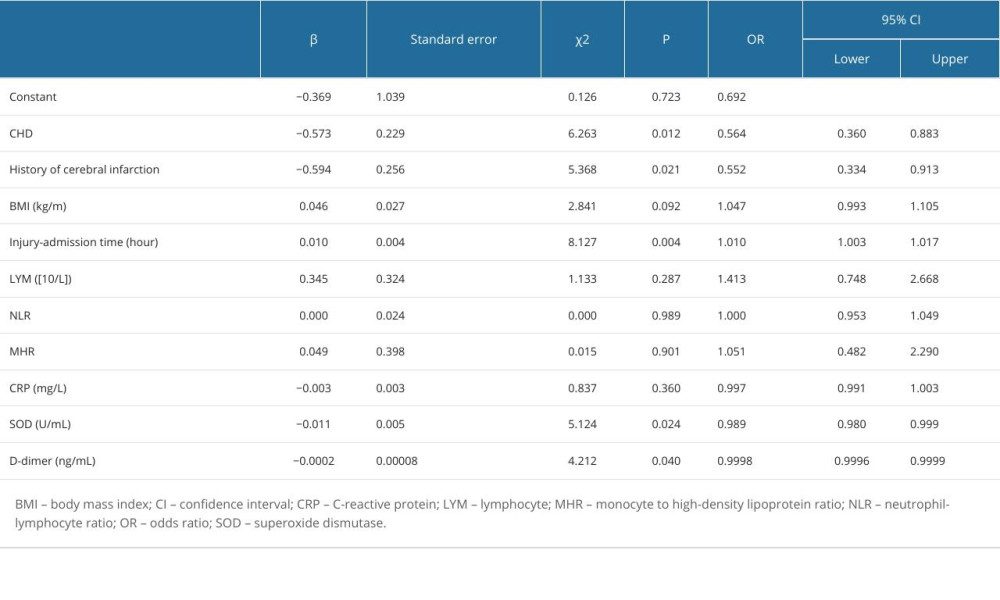 Table 3. Multivariate logistic regression analysis of DVT risk.
Table 3. Multivariate logistic regression analysis of DVT risk.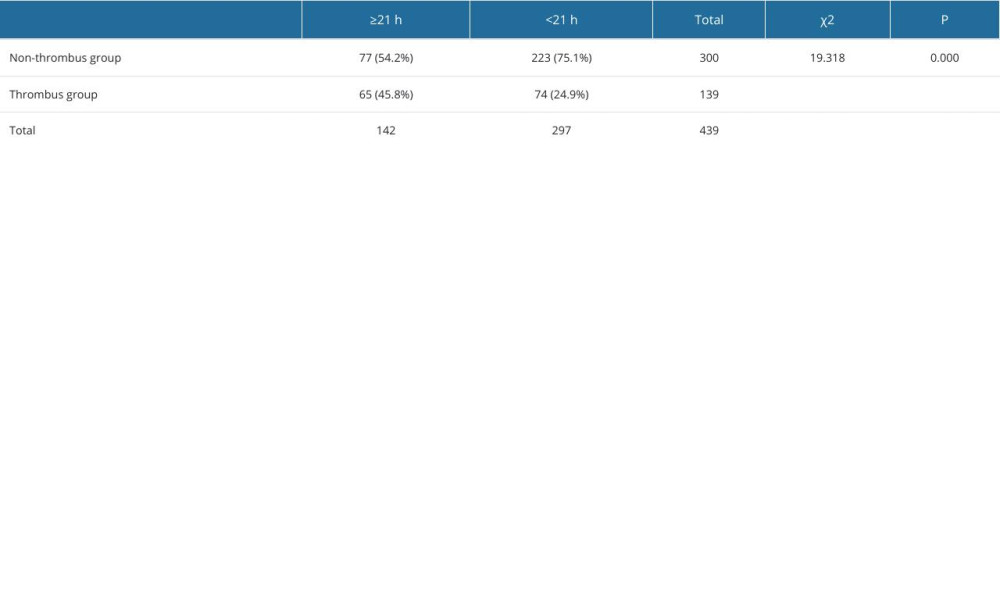 Table 4. Occurrence of thrombus according to the best cut-off value.
Table 4. Occurrence of thrombus according to the best cut-off value. In Press
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








