10 May 2024: Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Comparative Analysis with Median Thoracotomy
Hongbiao Ma1BCDEF, Qingjun Yang1BCDF, Rui Xiong1BCDF, Hao Chen1BCD, Yu Yan1BCD, Hongkun Wu1ACDEG*, Jieqiu Weng2BCFDOI: 10.12659/MSM.943089
Med Sci Monit 2024; 30:e943089
Abstract
BACKGROUND: One-lung ventilation is the separation of the lungs by mechanical methods to allow ventilation of only one lung, particularly when there is pathology in the other lung. This retrospective study from a single center aimed to compare 49 patients undergoing thoracoscopic cardiac surgery using one-lung ventilation with 48 patients undergoing thoracoscopic cardiac surgery with median thoracotomy.
MATERIAL AND METHODS: This single-center retrospective study analyzed patients who underwent thoracoscopic cardiac surgery based on one-lung ventilation (experimental group, n=49). Other patients undergoing a median thoracotomy cardiac operation were defined as the comparison group (n=48). The oxygenation index and the mechanical ventilation time were also recorded.
RESULTS: There was no significant difference in the immediate oxygenation index between the experimental group and comparison group (P>0.05). There was no significant difference for the oxygenation index between men and women in both groups (P>0.05). The cardiopulmonary bypass time significantly affected the oxygenation index (F=7.200, P=0.009). Operation methods (one-lung ventilation thoracoscopy or median thoracotomy) affected postoperative ventilator use time (F=8.337, P=0.005). Cardiopulmonary bypass time (F=16.002, P<0.001) and age (F=4.384, P=0.039) had significant effects on ventilator use time. There was no significant effect of sex (F=0.75, P=0.389) on ventilator use time.
CONCLUSIONS: Our results indicated that one-lung ventilation thoracoscopic cardiac surgery did not affect the immediate postoperative oxygenation index; however, cardiopulmonary bypass time did significantly affect the immediate postoperative oxygenation index. Also, one-lung ventilation thoracoscopic cardiac surgery had a shorter postoperative mechanical ventilation use time than did traditional median thoracotomy cardiac surgery.
Keywords: Cardiopulmonary Bypass, Hyperbaric Oxygenation, Thoracoscopy, Ventilators, Mechanical
Introduction
In the 1990s, Chitwood et al completed the world’s first thoracoscopic heart valve replacement operation, initiating the application of thoracoscopic technology in heart surgery [1]. Many heart operations, including valve replacement and valvuloplasty, require very precise operation [2]. Thoracoscopy can not only provide a stable and reliable light source, but can also help the surgeon accurately identify and separate various micro-tissues [3]. All of these advantages make the thoracoscopic treatment of valvular heart disease gradually accepted and recognized by an increasing number of people.
Minimally invasive thoracoscopic cardiac surgery has the advantages of a small incision, preservation of the integrity of the thorax, reduced postoperative pain, and rapid recovery [4]. Presently, many large and medium heart centers in China have conducted thoracoscopic cardiac surgery. According to preliminary statistics in 2016, there were more than 10 000 cases of thoracoscopic cardiac surgery in China [5]. A typical thoracoscopic cardiac surgery requires double lumen endotracheal intubation and one-lung ventilation outside of cardiopulmonary bypass, to ensure a good surgical field on the right side. One-lung ventilation has been shown to have a certain effect on lung function [6].
One-lung ventilation is the separation of the lungs by mechanical methods to allow ventilation of only one lung, particularly when pathology, such as malignancy, involves a single lung. One-lung ventilation has been proven to have a certain impact on lung function. Piccioni et al [7] reported that one-lung ventilation could result in a low incidence of acute respiratory distress syndrome and comparable postoperative complications in adult patients undergoing elective lung resection. The most common postoperative complications after cardiopulmonary bypass are pulmonary dysfunction and diseases of the respiratory system [8–10]. Questions remain, however, including whether one-lung ventilation and thoracoscopic cardiac surgery have a greater impact on lung function, and whether its associated postoperative pulmonary complications are more severe. Therefore, this retrospective study of a single center aimed to compare 49 patients undergoing thoracoscopic cardiac surgery using one-lung ventilation with 48 patients undergoing thoracoscopic cardiac surgery with median thoracotomy.
Material and Methods
ETHICS COMMITTEE APPROVAL:
This study was approved by the Ethics Committee of Chongqing General Hospital (approval No. S2019-033-01). All patients provided their written informed consent to participate in this study.
PATIENTS:
A total of 49 patients undergoing adult heart surgery with one-lung ventilation thoracoscopy in our hospital from January 5, 2018, to March 1, 2019, were selected as the experimental group (n=49). In addition, 48 patients undergoing adult heart operation with median thoracotomy in the same period were selected as the comparison group (n=48; Table 1). The one-lung ventilation thoracoscopic cardiac surgery and positive end-expiratory pressure were performed according to a previous study [11].
The inclusion criteria were as follows: (1) patients undergoing heart surgery (one-lung ventilation thoracoscopic cardiac surgery or median thoracotomy heart operation), and (2) patients with complete preoperative and postoperative data.
The exclusion criteria were as follows: (1) preoperative chronic obstructive pulmonary disease, preoperative arterial blood gas PO2 <60 mmHg; (2) grade IV preoperative cardiac function, left ventricular ejection fraction <35%; (3) difficulty in operation or cardiopulmonary bypass time >360 min; (4) reopening and hemostasis due to bleeding after the operation; (5) difficulty in postoperative rebound, low cardiac output syndrome, or use of auxiliary devices; and (6) conversion from thoracoscopic operation to median thoracotomy.
ANESTHESIA METHODS:
Anesthesia was induced by administering midazolam 1 to 2 mg, etomidate 0.3 mg/kg, atracurium cis-benzenesulfonate 0.15 mg/kg, and sufentanil 0.8 to 1.2 UG/kg. After induction, patients in the comparison group were placed on a single lumen trachea catheter, while the patients in the experimental group were placed on a double lumen trachea catheter (left branch), and depth was adjusted with a fiberbronchoscope. The right internal jugular vein was placed into a superior lumen drainage tube.
Anesthetization was performed by continually injecting 1% propofol at a dose of 2 mg/kg/h, and intermittently administering sufentanil, atracurium cis-benzenesulfonate, and inhaled sevoflurane to maintain the appropriate depth of anesthesia. After tracheal intubation, patients in both groups underwent intermittent positive pressure ventilation, with a tidal volume of 6 to 8 mL/kg, frequency of 10 to 12 times/min, inhaled oxygen concentration of 60%, and end-expiratory carbon dioxide partial pressure of 35 to 45 mmHg.
CARDIOPULMONARY BYPASS:
In the experimental group, the catheterization of the right jugular vein and catheterization of the femoral vein were used to drain the vena cava, and the catheterization of the femoral artery was used as an artery pump tube to block the superior and inferior vena cava in the pericardium. The comparison group was intubated by the superior and inferior vena cava and the ascending aorta in the pericardium to establish cardiopulmonary bypass, using a heart-lung machine system (LivaNova Deutschland GmbH, Germany) and membrane oxygenator (Medtronic, Inc, USA). In the experimental group, cardiopulmonary bypass was started before the incision of the open heart bag and stopped after the incision of the heart and chest wall completely stopped bleeding. In the comparison group, cardiopulmonary bypass was started and stopped. In both groups, 20 mg of dexamethasone was added before cardiopulmonary bypass, but no ulinastatin was used. The rapid BLS blood filter was used after shutdown.
Furthermore, during cardiopulmonary bypass, continuous positive airway pressure (5–10 cmH2O), or low tidal volume (3–5 mL/kg) plus low positive end-expiratory pressure (5 cmH2O) were applied to reduce the inflammatory response of the extracorporeal circulation and protect postoperative pulmonary function [12].
OPERATIVE METHODS:
In the experimental group, the right side was raised 15° to 20° in the supine position, and the endoscopic hole was located at the sixth intercostal space between the axillary front line. The main operation hole was located at the fourth intercostal space between the right clavicular midline and the axillary front line. The auxiliary operation hole was located at the fourth intercostal space between the axillary front line. For the comparison group, the sternum was split, and the pericardium was suspended to complete the operation.
OBSERVATION INDEX:
After the operation, the patients were transferred to the Intensive Care Unit (ICU), and the blood gas analysis data were recorded immediately and at 4 h, 8 h, 12 h, and 16 h after the operation. Then, the tracheal intubation was pulled out, and the use time of the ventilator was recorded. The ventilator was operated in the patients according to the weaning systems as the instrument instructions.
STATISTICAL ANALYSIS:
In this study, SPSS 21.0 software was used for analysis, and multivariate analysis of variance (ANOVA) was used to analyze the data. The biases and confounding factors were excluded with the logistic regression modeling method. A
Results
NO DIFFERENCES IN OXYGENATION INDEX WERE DISCOVERED BETWEEN THE EXPERIMENTAL AND COMPARISON GROUPS:
The results of the blood gas analysis showed that there was no significant difference in the immediate oxygenation index between the experimental group and the comparison group (Table 1, P>0.05). Meanwhile, in both the experimental group and comparison group, there were no significant differences in the immediate oxygenation index between men and women (Table 1, P>0.05).
CARDIOPULMONARY BYPASS TIME AFFECTED THE OXYGENATION INDEX:
The findings of the multivariate ANOVA indicated that the cardiopulmonary bypass time significantly affected the immediate oxygenation index after the operation (Table 2, F=7.200, P=0.009).
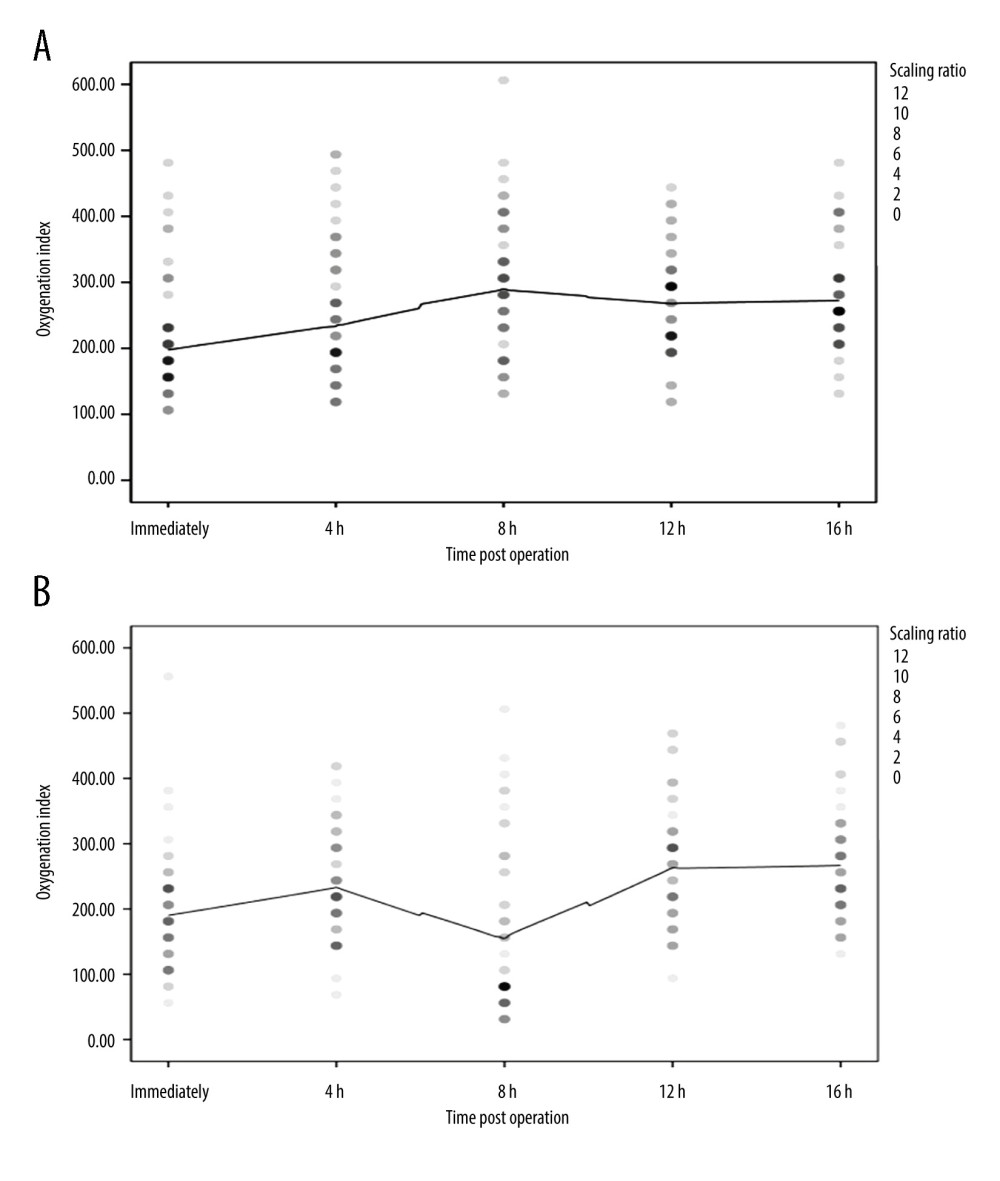
TREND OF FITTING CURVE OF POSTOPERATIVE OXYGENATION INDEX:
The fitting curve of the oxygenation index of the experimental group (Figure 1A) and the comparison group (Figure 1B) was drawn immediately, and at 4 h, 8 h, 12 h, and 16 h after surgery. According to the findings of the blood gas analysis, the curve indicated that the oxygenation index of the comparison group decreased at 8 h after the operation, while that of the experimental group increased slightly at 8 h after the operation; however, there were no statistically significant differences between the 2 groups (Figure 1, P>0.05).
INFLUENCE FACTORS FOR POSTOPERATIVE VENTILATOR USE TIME:
The results of ANOVA of postoperative ventilator use time showed that operation mode (experimental group and comparison group) significantly affected the postoperative ventilator use time (Table 3, F=8.337, P=0.005). The findings of ANOVA also showed that cardiopulmonary bypass time (Table 3, F=16.002, P=0.000) and age (Table 3, F=4.384, P=0.039) significantly affected the use of ventilator time after the operation. However, sex (Table 3, F=0.75, P=0.389) had no significant effect on ventilator use time.
Discussion
The present findings showed that there was no significant difference in the immediate oxygenation index between the experimental group and the comparison group and between men and women in both groups. Cardiopulmonary bypass time affected the oxygenation index. Operation methods (one-lung ventilation or median thoracotomy) affected postoperative ventilator use time. Cardiopulmonary bypass time and age significantly affected ventilator use time. However, there was no significant effect of sex on ventilator use time. The one-lung ventilation thoracoscopic cardiac surgery demonstrated better clinical outcomes than did traditional median thoracotomy cardiac surgery.
With the development of minimally invasive thoracoscopic surgery, thoracoscopic technology has been widely used in lobectomy, esophageal surgery, mediastinal surgery, and heart surgery [13]. One-lung ventilation is usually needed in thoracoscopic surgery, providing a good operating field and operating space, especially for heart surgery. When thoracoscopic single-lung ventilation is used to cut open the heart bag, the right lung collapses as well, which can avoid damaging the lung tissue. After cardiopulmonary bypass, complete hemostasis is the key to the operation of the whole heart. Good right lung collapse can help doctors thoroughly check and stop bleeding. One-lung ventilation is the exposure to thoracic surgery through double lumen endotracheal intubation or a bronchial blocker. During one-lung ventilation, the collapsed side of the lung will lack oxygen due to the lack of ventilation and oxygen exchange. However, hypoxia will lead to pulmonary vasoconstriction and the flow from the collapsed side will flow to the ventilating side. The results showed that the pulmonary blood flow on the operative side represented 40% of the total pulmonary blood flow and the pulmonary blood flow on the ventilating side represent 60% [14]. As a result of hypoxia and a series of inflammatory interstitial reactions, the flow of the collapsed side of the lung is diverted by at least 40% to 50% to the pulmonary vessels on the ventilating side to correct the state of hypoxia [15]. The mechanism of one-lung ventilation on lung injury is complex and multifactor [9]. The question of how to reduce lung injury caused by one-lung ventilation has always been the focus of research on one-lung ventilation [16]. The lung protection method of one-lung ventilation is still improving. Some researchers have proposed that the pressure control ventilation mode is better than the volume control mode when one-lung ventilation is used [17]. Some researchers also suggested that when one-lung ventilation is used, the oxygen catheter is put into the collapsed side of the lung, and the oxygen input lasts for 3 L/min, which will obviously improve the hypoxic attack during the operation and reduce postoperative lung complications [12].
Although cardiopulmonary bypass materials continue to improve, acute lung injury after cardiopulmonary bypass is still the most common complication [18]. The clinical manifestations of postoperative pulmonary dysfunction are atelectasis, pleural effusion, lower respiratory tract infection, symptomatic or asymptomatic hypoxemia, and adult respiratory distress syndrome. According to some reports, the rate of pulmonary complications after cardiopulmonary bypass ranges from 10% to 25% [19,20]. One study [21] showed that even in cardiopulmonary bypass without severe cardiac dysfunction, postoperative pulmonary function will continue to be affected for weeks or longer. The incidence of adult respiratory distress syndrome after cardiopulmonary bypass is as high as 0.6% to 20%. Once adult respiratory distress syndrome occurs, the mortality rate is as high as 80% [22]. Similarly, 43% of patients who returned to the ICU after cardiopulmonary bypass return due to postoperative respiratory dysfunction [23]. The causes of lung injury in cardiopulmonary bypass include the following: lung injury caused by cardiopulmonary bypass, lung injury caused by blood transfusion, lung injury caused by mechanical ventilation, and lung injury caused by cardiac insufficiency. During cardiopulmonary bypass, a series of factors, such as hemodilution, excessive volume load, hypoxia, systemic heparinization, continuous non-pulsating blood flow, and blood contact with the surface of the external pipeline, will activate the cascade of human inflammatory media, produce a large number of inflammatory media, and affect postoperative pulmonary function [24,25]. Less postoperative volume load is helpful for the recovery of lung function [26]. During cardiopulmonary bypass, the complete disconnection of mechanical ventilation can well expose the field of cardiac surgery. However, during cardiopulmonary bypass, 5 to 10 cmH2O of continuous positive airway pressure or low tidal volume of 3 to 5 mL/kg plus low positive end-expiratory pressure of 5 cmH2O can reduce the inflammatory response of extracorporeal circulation and protect postoperative lung function [12]. Mechanical ventilation before and after cardiopulmonary bypass can also significantly affect pulmonary function after cardiac surgery. A previous study [27] showed that protective mechanical ventilation strategies with low intraoperative volume of 6 to 8 mL/kg, positive end-expiratory pressure, lung recruitment technique, and an air oxygen ratio (FiO2) less than 80% can significantly reduce surgery mortality, incidence of postoperative pulmonary complications, and postoperative hospital stay.
In the present study, the factors influencing lung function after minimally invasive heart surgery with one-lung ventilation and cardiopulmonary bypass were observed. The results showed that cardiopulmonary bypass time had a significant effect on the oxygenation index of blood gas (
This study had some limitations. First, the diffusing capacity of the lung for carbon monoxide was not performed before and after surgery in the lung examination laboratory to obtain full assessment of the gas exchange. Second, one-lung ventilation thoracoscopic cardiac surgery, although it does not change oxygen parameters, may cause changes in lung tissue, which is observed in postoperative imaging and results from the surgical technique, manipulation, and compression of the lung tissue causing local perfusion problems. However, this study did not determine lung injury, such as with postoperative lung X-ray examination. Third, there are no data on surgical treatment and postoperative complications. Fourth, we attempted to reduce the biases and confounding factors with the logistic regression modeling method. However, we involved only a few potential exposure factors when modeling, which may have affected the reduction of biases and confounding factors. Fifth, in this study, it is hard to determine if just a median thoracotomy causes enough damage to cause the above results rather than just single lung ventilation being as adequate. In future investigations, we will conduct an investigation to clarify the effects of median thoracotomy and one-lung ventilation on lung functions.
Conclusions
This study showed that one-lung ventilation thoracoscopic cardiac surgery did not affect the immediate postoperative oxygenation index; however, cardiopulmonary bypass time did significantly affect the immediate postoperative oxygenation index. At the same time, one-lung ventilation thoracoscopic cardiac surgery demonstrated a shorter postoperative mechanical ventilation time than did traditional median thoracotomy cardiac operation. Therefore, one-lung ventilation thoracoscopic cardiac surgery could improve lung function after the operation. We will endeavor to improve the operative process of one-lung ventilation thoracoscopic cardiac surgery and increase its clinical application.
References
1. Chitwood WR, Elbeery JR, Chapman WH, Video-assisted minimally invasive mitral valve surgery: The “micro-mitral” operation: J Thorac Cardiovasc Surg, 1997; 113; 413-14
2. Sheng W, Qiao H, Niu Z, Prospective study on the postoperative use of levosimendan after conventional heart valve replacement: Med Sci Monit, 2021; 27; e932001
3. Lan L, Cen Y, Zhang C, A propensity score-matched analysis for non-intubated thoracic surgery: Med Sci Monit, 2018; 24; 8081-87
4. Aalaei-Andabili SH, Miles WM, Burkart TA, Minimally invasive thoracoscopic surgery is an effective approach for treating inappropriate sinus tachycardia: J Cardiovasc Electrophysiol, 2019; 30; 1297-303
5. Li J, Liu H, Liu J, Challenges in complex video-assisted thoracoscoic surgery and spontaneous respiration video-assisted thoracoscopic surgery procedures: J Vis Surg, 2017; 3; 31
6. Senturk M, Slinger P, Cohen E, Intraoperative mechanical ventilation strategies for one-lung ventilation: Best Pract Res Clin Anaesthesiol, 2015; 29; 357-69
7. Piccioni F, Langiano N, Bignami E, One-lung ventilation and postoperative pulmonary complications after major lung resection surgery. A multicenter randomized controlled trial: J Cardiothorac Vasc Anesth, 2023; 37; 2561-71
8. Huffmyer JL, Groves DS, Pulmonary complications of cardiopulmonary bypass: Best Pract Res Clin Anaesthesiol, 2015; 29; 163-75
9. Lohser J, Slinger P, Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung: Anesthesia Analgesia, 2015; 121; 302-18
10. Ashok V, Francis J, A practical approach to adult one-lung ventilation: BJA Educ, 2018; 18; 69-74
11. Zhang Y, Yan W, Fan Z, Preemptive one lung ventilation enhances lung collapse during thoracoscopic surgery: A randomized controlled trial: Thorac Cancer, 2019; 10; 1448-52
12. Jung DM, Ahn HJ, Jung SH, Apneic oxygen insufflations decrease the incidence of hypoxemia during one-lung ventilation in open and thoracoscopic pulmonary lobotomy: A randomized controlled trail: J Thorac Cardiovasc Surg, 2017; 154; 360-36
13. Purohit A, Bhargava S, Mangal V, Parashar VK, Lung isolation, one-lung ventilation and hypoxaemia during lung isolation: Indian J Anaesthesia, 2015; 9; 606-17
14. Schilling T, Kozian A, Senturk M, Effect of volatile and intravenous anesthesia on the alveolar and systemic inflammatory response in thoracic surgical patients: Anesthesiology, 2011; 115; 65-74
15. De Conno E, Steurer MP, Wittlinger M, Anesthetic-induced improvement of the inflammatory response to one-lung ventilation: Anesthesiology, 2009; 110; 1316-26
16. Meleiro H, Correia I, Charco Mora P, New evidence in one-lung ventilation: Revista Espanola de Anestesiologia Y Reanimacion, 2018; 65; 149-53
17. Zhu YQ, Fang F, Ling XM, Pressure-controlled versus volume-controlled ventilation during one-lung ventilation for video-assisted thoracoscopic lobectomy: J Thorac Dis, 2017; 9; 1303-9
18. Wang YC, Huang CH, Tu YK, Effects of positive airway pressure and mechanical ventilation of the lungs during cardiopulmonary bypass on pulmonary adverse events after cardiac surgery: A systematic review and meta-analysis: J Cardiothorac Vasc Anesth, 2018; 32; 748-59
19. Hulzebos EH, Helders PJ, Favié NJ, Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: A randomized clinical trail: JAMA, 2006; 296; 1851-57
20. Zarbock A, Mueller E, Netzer S, Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: A prospective, randomized, controlled trail in 500 patients: Chest, 2009; 135; 1252-59
21. Landoni G, Mizzi A, Biondi-Zoccai G, Reducing mortality in cardiac surgery with levosimendan: A meta-analysis of randomized controlled trials: J Cardiothorac Vasc Anesth, 2010; 24; 51-57
22. Kogan A, Preisman S, Levin S, Adult respiratory distress syndrome following cardiac surgery: J Cardiac Surg, 2014; 29; 41-46
23. Jarząbek R, Bugajski P, Greberski K, Readmission to an intensive care unit after cardiac surgery: Reasons and outcomes: Kardiol Pol, 2014; 72; 740-47
24. Day JRS, Taylor KM, The systemic inflammatory response syndrome and cardiopulmonary bypass: Int J Surg, 2005; 33; 129-40
25. Warren OJ, Watret AL, de Wit KL, The inflammatory response to cardiopulmonary bypass: part II-Anti-inflammatory therapeutic strategies: J Cardiothorac Vasc Aneth, 2009; 23; 284-92
26. Kosour C, Dragosavac D, Antunes N, Effect of ultrafiltration on pulmonary function and interleukins in patients undergoing cardiopulmonary bypass: J Cardiothoracic Vasc Anesthesia, 2016; 30; 884-90
27. Ferrando C, Soro M, Beida FJ, Protection strategies during cardiopulmonary bypass: ventilation, anesthetics and oxygen: Curr Opin Anesthesiol, 2015; 28; 73-80
28. Ogut S, Sucu Dag G, Pain characteristics and pain interference among patients undergoing open cardiac surgery: J Perianesth Nurs, 2019; 34; 757-66
29. Marongiu I, Spinelli E, Mauri T, Cardio-respiratory physiology during one-lung ventilation: complex interactions in need of advanced monitoring: Ann Transl Med, 2020; 8; 524
Tables
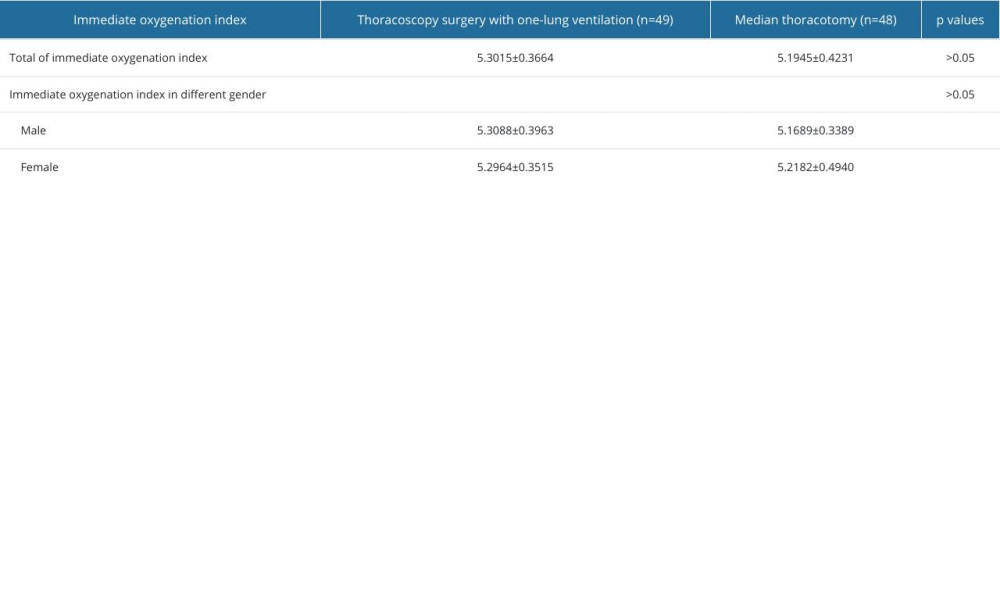 Table 1. Effects of sex and operative methods on immediate oxygenation index.
Table 1. Effects of sex and operative methods on immediate oxygenation index.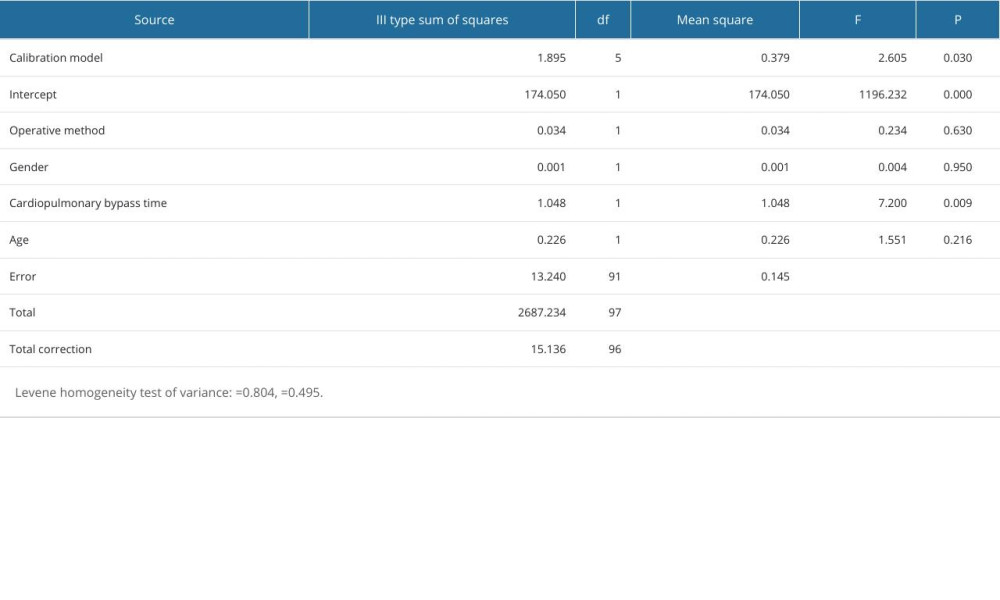 Table 2. Findings for multivariate analysis of variance of immediate oxygenation index after operation.
Table 2. Findings for multivariate analysis of variance of immediate oxygenation index after operation.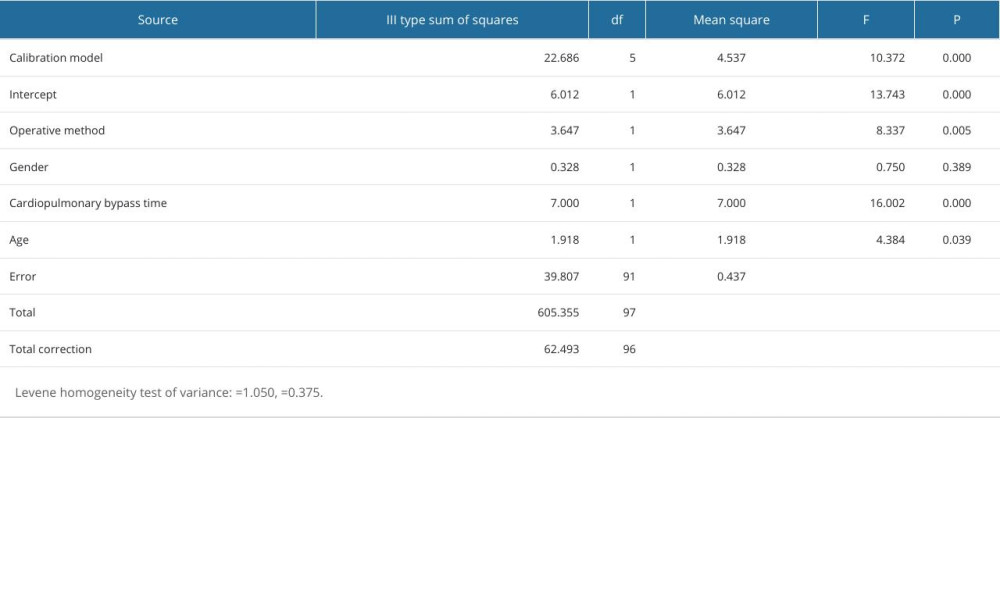 Table 3. Multivariate analysis of variance of ventilator use time.
Table 3. Multivariate analysis of variance of ventilator use time.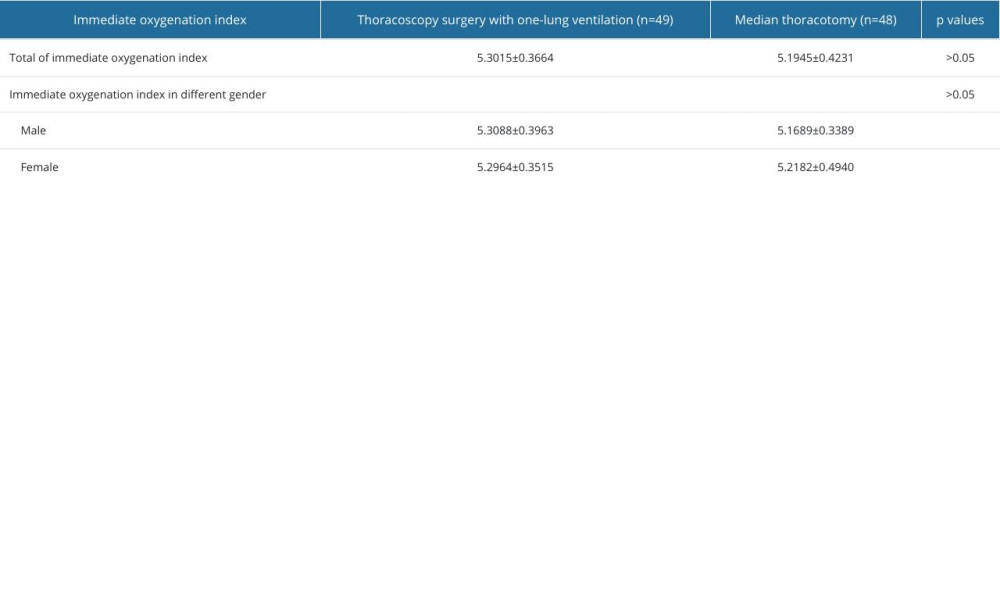 Table 1. Effects of sex and operative methods on immediate oxygenation index.
Table 1. Effects of sex and operative methods on immediate oxygenation index.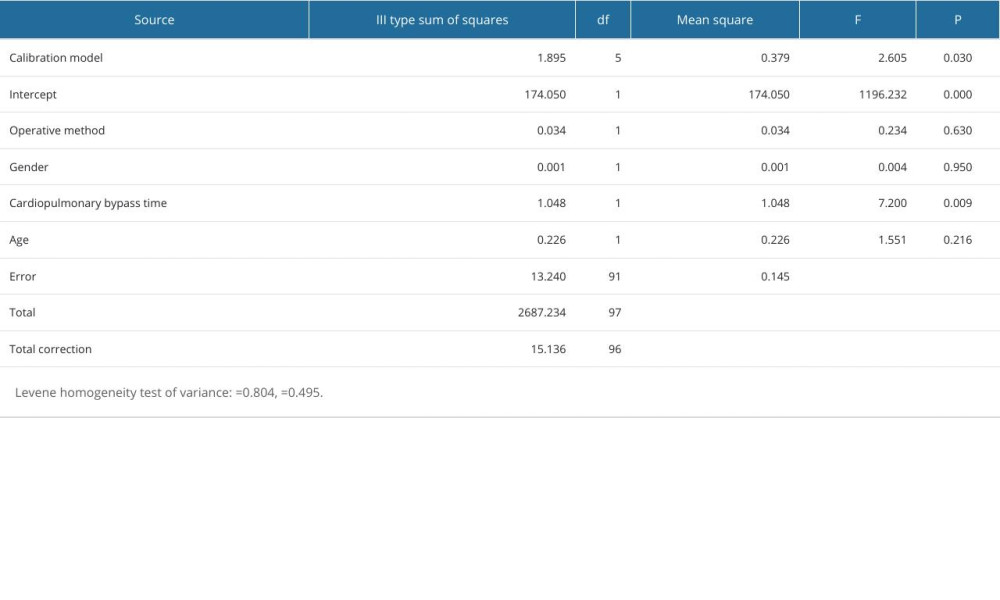 Table 2. Findings for multivariate analysis of variance of immediate oxygenation index after operation.
Table 2. Findings for multivariate analysis of variance of immediate oxygenation index after operation.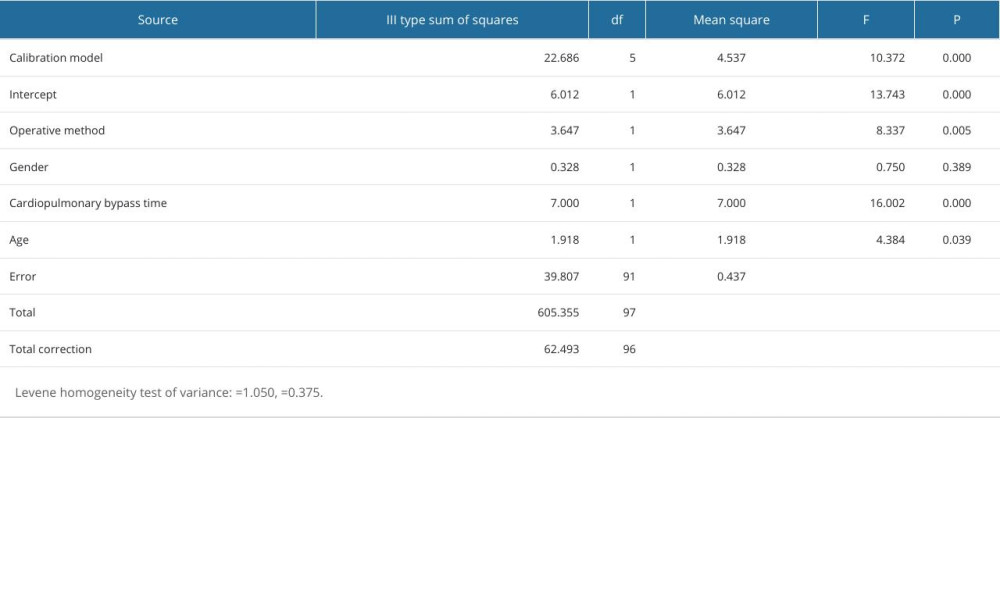 Table 3. Multivariate analysis of variance of ventilator use time.
Table 3. Multivariate analysis of variance of ventilator use time. In Press
07 May 2024 : Clinical Research
Treatment of AVN-Induced Proximal Pole Scaphoid Nonunion Using a Fifth and Fourth Extensor Compartmental Ar...Med Sci Monit In Press; DOI: 10.12659/MSM.944553
16 Mar 2024 : Clinical Research
Diagnostic Efficiency of ACR-TIRADS Score for Differentiating Benign and Malignant Thyroid Nodules of Vario...Med Sci Monit In Press; DOI: 10.12659/MSM.943228
08 May 2024 : Clinical Research
Effect of Individualized PEEP Guided by Driving Pressure on Diaphragm Function in Patients Undergoing Lapar...Med Sci Monit In Press; DOI: 10.12659/MSM.944022
21 Mar 2024 : Clinical Research
Impact of Serum Vitamin D, B6, and B12 and Cognitive Functions on Quality of Life in Peri- and Postmenopaus...Med Sci Monit In Press; DOI: 10.12659/MSM.943249
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952