24 March 2024: Clinical Research
Psychological and Physical Well-Being in Women Diagnosed with Breast Cancer: A Comprehensive Study of Anxiety, Depression, Sleep Quality, Physical Activity, and Sociodemographic Factors
Oliver J. CzechDOI: 10.12659/MSM.943490
Med Sci Monit 2024; 30:e943490
Abstract
BACKGROUND: The psychophysical state of breast cancer patients impacts several outcomes and parameters and can directly affect diagnosis, prehabilitation, and treatment. This questionnaire-based study aimed to compare anxiety levels, depression, physical activity, sleep quality, and sociodemographic features in women with breast cancer and healthy women at a breast cancer unit in Poland.
MATERIAL AND METHODS: The study enrolled 41 breast cancer patients with no proposed treatment or psychological disorder diagnosis and 50 healthy volunteers. After enrolment, the subjects completed the Spielberger State-Trait Anxiety Inventory (STAI), Beck’s Depression Inventory (BDI), International Physical Activity Questionnaire (IPAQ), Pittsburgh Sleep Quality Index (PSQI), and a sociodemographic questionnaire.
RESULTS: In this study, anxiety levels measured by the STAI anxiety subscale (56.05 [9.18] vs 37.62 [8.35], P<0.001) and BDI-assessed depression levels were higher in the cancer group (12.34 [6.26] vs 6.68 [6.36], P<0.001). PSQI measured quality of sleep (QOS) (5.80 [3.44] vs 3.76 [3.35], p=0.003) and physical activity (PA) levels evaluated by IPAQ were lower for breast cancer patients (1684.62 [2401.19] vs 3473.44 [4756.78], P=0.042).
CONCLUSIONS: Anxiety, depression, poor quality of sleep, and insufficient PA were common in breast cancer patients. The occurrence of cancer was the main factor causing mental health deterioration in patients with breast cancer. Also, mental state and well-being differed in healthy women compared to breast cancer patients.
Keywords: Medical Oncology, Neoplasms, Preoperative Exercise, Behavioral Symptoms, Emotions
Introduction
According to statistical data, neoplasms are the second leading cause of death and disability after cardiac diseases and cause around 270 000 deaths annually in Europe [1]. Globally, mortality and morbidity rates are similar, but one issue remains unchanged – cancer incidence is increasing worldwide and is projected to become the leading cause of death after 2030 [2]. Currently, cancer seems to be particularly important due to its health, economic, and general well-being consequences. Therefore, it seems necessary to react to the situation by strengthening therapeutic management strategies. The most common cancer in females is malignant breast cancer [3].
The diagnosis of breast cancer can become a mentally taxing event, and coping can be very challenging [4]. Levels of mental distress are often very high immediately after diagnosis [5,6]. At this stage, fear of the future becomes the main concern, as shown in many after cancer diagnosis [7,8]. Worries about the prognosis of the disease, experiencing pain, and suffering from cancer therapies increase the levels of general distress in terms of anxiety, depression, and anger [9,10].
Many patients have access to extensive information on the internet and attempt to follow their own ideas about their health, which are not usually in line with the facts. For example, modern methods are used as additional cancer treatments, which allows the fight against breast cancer to be less devastating than in the past [11].
Unfortunately, there are still no treatments devoid of adverse effects [12]. Nonetheless, thanks to novel mechanisms of action and supplementary therapies, there is an increased supply of targeted chemotherapeutic drugs that increase the effectiveness of breast cancer treatment [13–15] but also cause a greater risk of fatigue, reduced patient quality of life (QOL), psychological distress, and physical functioning. Such knowledge is available to cancer patients and often leads to stress, fear, and anxiety, and generally affects their QOL, even at the time of diagnosis [16].
Since breast cancer diagnosis relates more and more to young, socially active women, the ways of dealing with the diagnosis are also radically different [17]. One of the symptoms partially caused by stress, anxiety, and fear is deteriorating quality of sleep (QOS). An inappropriate balance of rest and activity, combined with multiplying disorders of psychophysical well-being and the development of the disease, can contribute to the occurrence and deepening of depressive states [17]. A study by Torrisi et al showed that depressive states can influence the overall QOL [18]. Such a large variety of symptoms means that oncological standards of care, from the diagnosis to the end of the healing process, require an interdisciplinary approach and holistic treatment methods, which cover much broader symptomatology than the tumor itself [19].
Numerous factors can positively affect oncology patient QOL and psychometric condition at the diagnosis stage [20,21]. Oncology departments usually offer psychological support to patients at every stage of the disease. An additional positive factor influencing QOL is the high overall integration and social activity of oncology patients. Patients at various stages of diagnosis and disease often associate in cancer patient clubs and exchange their experiences and observations [22]. Another factor influencing the mental well-being of cancer patients is their familial status. Indeed, Krok et al showed a correlation between marital status and the ability to cope with the disease [23].
Physical activity (PA) is also very important for breast cancer prevention and prognosis. Sun et al [24] investigated the benefits of PA for breast cancer patient QOL, anxiety, and depression, strongly concluding that PA was an effective intervention for QOL improvement and in reducing anxiety in participants, and showed positive trends in lowering depression symptoms. PA, kinesiotherapy, exercise training, and other types of movement are important in lowering the epidemical risk for breast cancer. Researchers agree that it is not only important whether a person is active, but the amount and intensity of all PA also plays a significant role. According to Diao et al [25], individuals with high levels of activity (above 8000 MET [metabolic equivalent]-minutes/week) had a 10.3% reduction of breast cancer occurrence risk compared with participants with insufficient activity (below 600 MET-minutes/week).
Therefore, this questionnaire-based study aimed to compare anxiety levels, depression, physical activity, sleep quality, and sociodemographic features in women with breast cancer and healthy women at a breast unit in Poland. The hypotheses were as follows: H1 - Patients with breast cancer diagnosis exhibit higher levels of anxiety and depression compared to healthy individuals; H2 - Healthy participants differ from patients after breast cancer diagnosis in terms of QOS and levels of PA; and H3 - Breast cancer diagnosis, QOS, level of PA, and patient age will serve as significant predictors of the intensity of psychological symptoms.
Material and Methods
PARTICIPANTS AND RECRUITMENT:
The Ethics Committee of the University School of Physical Education in Wrocław, Poland, approved the study (number 18/2019), which followed the guidelines of the Declaration of Helsinki. All participants gave written consent for study enrolment and medical data transfer. The consent process was prepared with the hospital’s Personal Data Inspector. The study enrolled 91 participants divided into 2 group: a “diagnosis group” (DG) and a “healthy group” (HG). Inclusion criteria for both groups were as follows: female gender, aged 40–65 years, no mental or cognitive deficits that could affect the research result, and written consent to participate in the research. Additionally, in the DG, we included patients with breast cancer as the primary diagnosis and no treatment proposed yet, and the exclusion criterion was the presence of a serious internal medical condition that could be a reason for changing the current lifestyle. The DG included 41 breast cancer patients from the cohort diagnosed with breast cancer, from the Lower Silesian Oncology, Pulmonology, and Hematology Center, Wrocław, Poland. Patients were randomly enrolled in the study after meeting the inclusion criteria. Patients were included in the study at the time of diagnosis prior to the multidisciplinary team (MDT) meeting.
MEASUREMENTS:
The participants completed a sociodemographic questionnaire, providing basic personal information and educational (education level), residential and financial status (4-point Likert scale), and marital status. Additionally, for participants in the DG, information such as estrogen receptor expression, progesterone receptor expression, human epidermal growth factor receptor 2 (HER2)-positive breast cancer, Ki-67 proliferation index >25%, and clinical tumor node metastasis (cTNM) cancer staging were retrieved. The participants in both groups completed 4 standardized questionnaires, according to anxiety and depression levels, PA assessment, and evaluation of QOS.
STATE-TRAIT ANXIETY INVENTORY:
The Spielberger State-Trait Anxiety Inventory (STAI) is a 40-item self-reported questionnaire measuring anxiety as a state and a trait, with 20 items each. Only 1 of the subscales was used for assessment (assessment of anxiety as a state, STAI-X1). This part of the questionnaire is a highly sensitive tool, which shows dynamics of anxiety, even in small time intervals. The inventory contains statements relating to current mood (eg, tension, nervousness, worrying, concerns). Items are rated on a 4-point scale, with higher scores indicating severe anxiety [26]. The inventory was developed to measure an individual’s tendency to experience anxiety. The occurrence of anxiety in cancer treatment has been repeatedly confirmed. Using this tool, it is intended to determine the extent to which a diagnosis of breast cancer affects the level of anxiety as a chronic condition.
BECK DEPRESSION INVENTORY:
Beck’s Depression Inventory (BDI) allows the assessment of depression levels and is a relevant psychometric tool with high reliability, the capacity to discriminate between depressed and non-depressed patients, and improved concurrent, content, and structural validity. It is a test commonly used in epidemiological studies as a screening test in the general population and in groups of patients with multiple diseases. The questionnaire contains 21 items covering cognitive-affective and somatic symptoms accompanying mood disorders. A sum score of 0–10 is a normal result, 11–26 indicates mild depressive symptoms, and 27+ indicates clinical depression. Higher total scores indicate more severe depressive symptoms [27]. Using this tool, it is possible to determine whether emotions related to a cancer diagnosis may constitute the basis for depressive states.
INTERNATIONAL PHYSICAL ACTIVITY QUESTIONNAIRE:
The International Physical Activity Questionnaire (IPAQ) examined patient PA levels. The scale was designed to estimate PA and sedentary behaviors in adults and consists of 7 questions regarding activities over the previous 7 days, based on 5 domains: (1) occupational PA; (2) transportation PA; (3) housework, house maintenance, and caring for the family; (4) recreation, sport, and leisure-time; and (5) time spent sitting. The questions concern the number of days and duration of intense and moderate PA, the frequency and length of walking, as well as the daily amount of time spent sitting. The questionnaire considers continuous activity lasting at least 10 minutes. Each domain allows assessment of the average time, quantity, and intensity of PA. PA is expressed in metabolic equivalent (MET)-min/week units in the IPAQ scale, which classifies respondents into 1 of 3 categories of activity: insufficient (less than 600), sufficient (600–1500 or 600–3000), or high (more than 1500 or 3000 MET-min/week) [28]. As physical activity is usually a parameter that results from habits, the use of this questionnaire allows assessment of the average activity level of study participants. Information about activity may provide knowledge about the epidemiology of breast cancer and will allow examination of the relationship between the level of activity and psychophysical well-being.
PITTSBURGH SLEEP QUALITY INDEX:
Participants’ QOS was assessed using the Pittsburgh Sleep Quality Index (PSQI). The PSQI is an efficient scale for measuring QOS and patterns and contains 19 self-reported items. Due to its brief and clinically useful assessment of many sleep disorders, this scale is widely used both in everyday practice and in clinical research. It assesses QOS in 7 categories: (1) subjective QOS, (2) sleep latency, (3) sleep duration, (4) habitual sleep efficiency, (5) sleep disturbances, (6) use of sleeping medication, and (7) daytime dysfunction. Each item is scored on a 4-point scale, and the global index score is calculated by totaling the 7 category scores to provide an overall score ranging from 0 to 21, where a lower score denotes better QOS. The sleep assessment covers the 1 month prior to the examination. The questionnaire has satisfactory psychometric aspects and high reliability (Cronbach’s alpha 0.83) [29]. Like physical activity, proper rest is the foundation of a healthy lifestyle. Assessing participants’ sleep quality allows examination of its impact on psychophysical parameters.
STATISTICAL ANALYSIS:
All analyses were conducted using JASP version 0.18.1 (University of Amsterdam, the Netherlands). Continuous variables are expressed as mean and standard deviation (SD), while categorical variables are presented as frequencies and percentages. Prior to analysis, the normality of the data distribution was assessed using the Shapiro-Wilk test. The unpaired t test or Mann-Whitney U test was employed to investigate differences between continuous variables, and a chi-squared χ2) test was used for categorical variables. Multiple linear regression (hierarchical) was utilized to determine the variables predicting the prevalence of depression and anxiety symptoms. The independent variables included breast cancer (disease occurrence), level of PA, sleep efficacy, age, and clinical outcomes (ie, estrogen receptor expression, progesterone receptor expression, and HER2-positive). The selection of variables results from available scientific reports, precisely described and summarized in a recent meta-analysis [30]. In all analyses, statistical significance was set at P<0.05. The statistical power of tests was calculated using G*Power software version 3.1 (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) according to studies assessing the effect size of the mentioned methods [31–34].
Results
PARTICIPANTS:
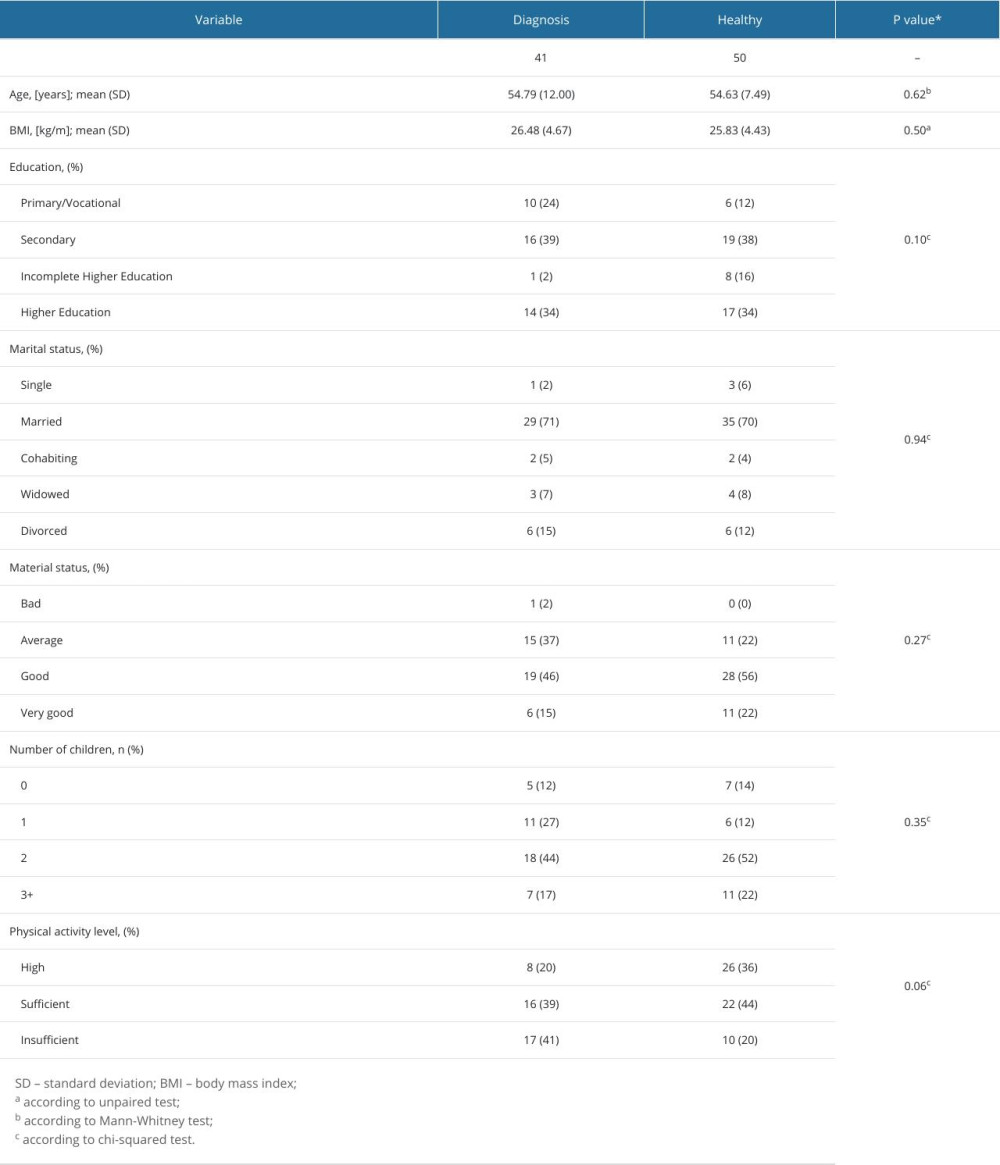
The study included 91 participants, with 41 in the DG and 50 in the HG, respectively. Sociodemographic characteristics are detailed in Table 1. Participants in both groups showed no significant differences in terms of age, body mass index (BMI), education, marital status, material status, and number of births. The only statistically significant difference between groups was observed in residential status (P=0.02).
DIAGNOSIS GROUP:
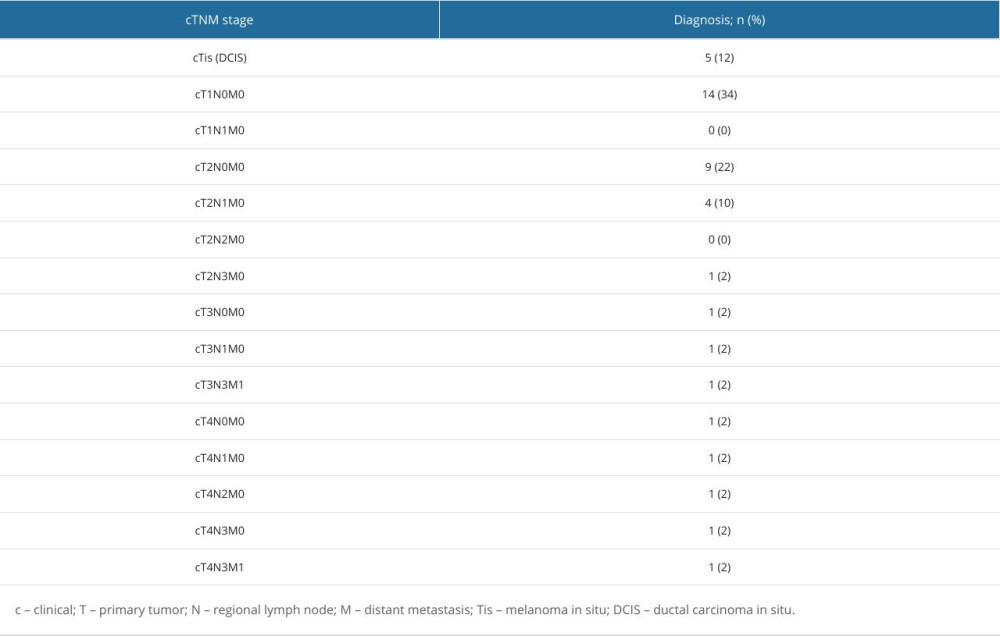
Estrogen receptor expression was detected in 88% of patients in the DG, while progesterone receptor expression was observed in nearly 80% of DG participants. HER2-positive breast cancer was identified in 20% of DG patients. A Ki-67 proliferation index >25% was present in the DG. The group characteristics, based on clinical tumor node metastasis (cTNM) cancer staging, are presented in Table 2.
RESULTS FOR PRIMARY OUTCOMES:
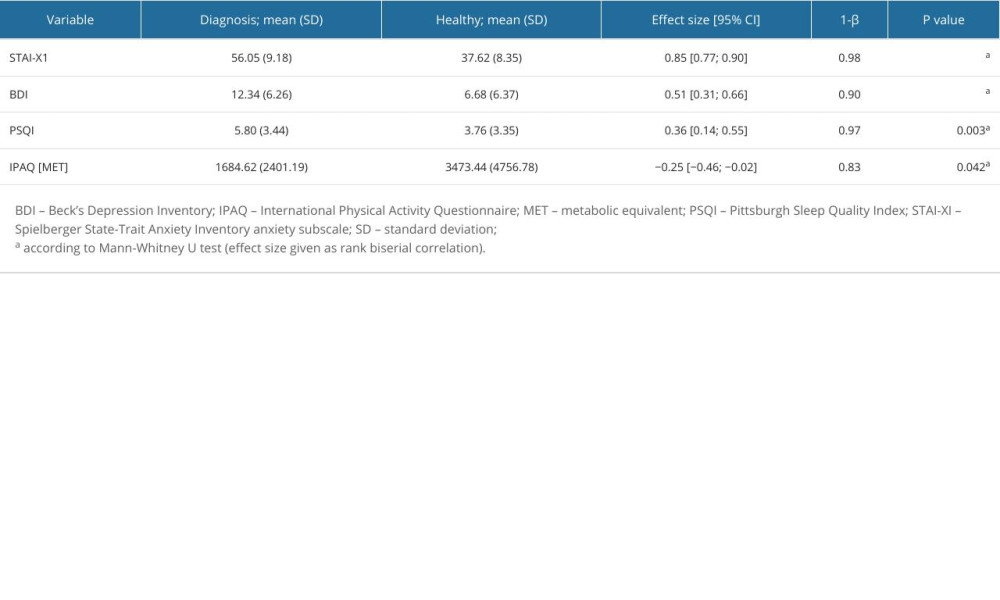
Table 3 presents detailed means and SD for the DG and HG. The results suggest that the psychophysical condition of patients in the HG is better compared to the DG in terms of the analyzed parameters. Anxiety levels were higher in the DG (56.05 [9.18] vs the HG 37.62 (8.35) (P<0.001)), and depression levels were also higher in the DG (12.34 [6.26] vs 6.68 [6.36]) (P<0.001). QOS was lower in the DG (3.76 [3.35] vs 5.80 [3.44]) (P=0.003), and PA levels were lower in the DG (1684.62 [2401.19] vs 3473.44 [4756.78]) (P=0.042). All measured parameters showed significant differences between groups.
FACTORS FOR PREDICTING DEPRESSION AND ANXIETY LEVEL:
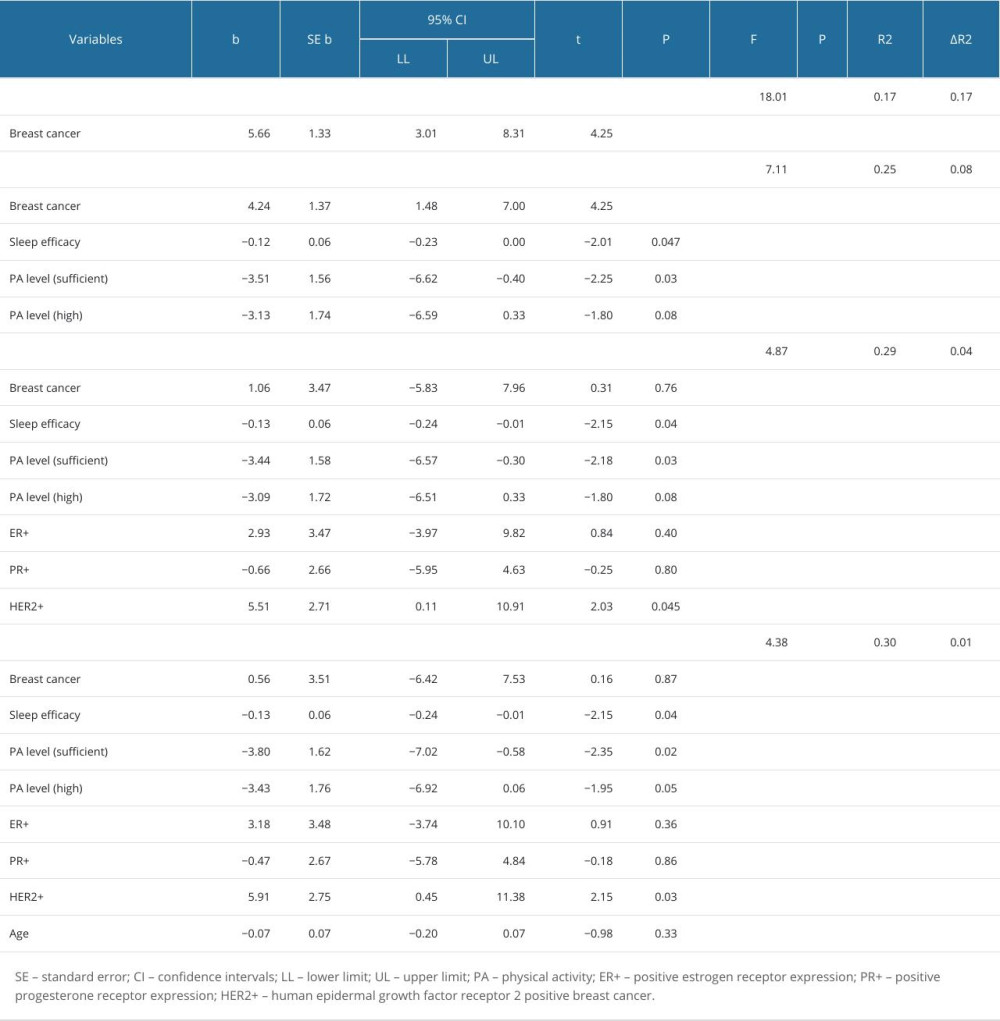
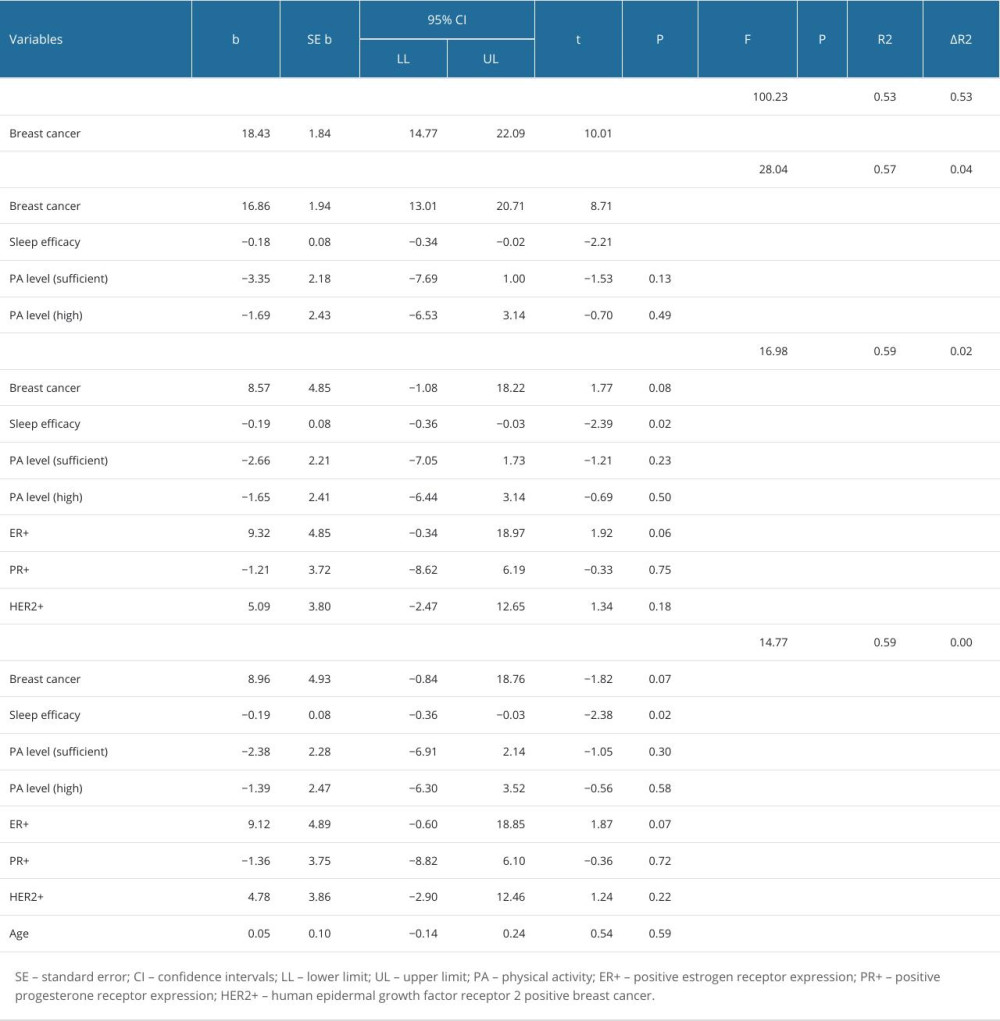
To explore the extent to which various factors contribute to the explanation of depression levels, a four-step hierarchical multiple regression was employed. The variables were chosen according to results of a recent meta-analysis [30]. The study design assumed it was necessary to investigate the contribution of the most common factors in the genesis of symptoms of anxiety and depression, which are one of the most frequently described effects of cancer on psychophysical health. We decided to perform a regression analysis and assess to what extent the diagnosis and stage of the disease, hormonal factors, and factors describing quality of life (eg, quality of sleep and physical activity) contribute to development of depression and anxiety. In the initial step, the occurrence of breast cancer emerged as a significant predictor variable, explaining 17% of the variance in depression (P<0.001). The second step introduced lifestyle factors, including sleep efficacy and PA level, all of which proved to be significant predictors, and there was no significant difference between sufficient and high PA levels. This expanded model accounted for 25% of the variance in depression (P<0.001). In the third step, clinical outcomes (estrogen receptor expression, progesterone receptor expression, and HER2-positive) were examined. In the third step, sleep efficacy, sufficient PA level, and HER2-positive emerged as significant predictor variables, explaining 30% of the variance in depression (P<0.001). In the fourth step, age was added to the regression model, and no changes in significant predictors were found. The fourth model explains about 30% of the depression variance (P<0.001) (Table 4).
To investigate the factors contributing to anxiety levels, a four-step hierarchical multiple regression was utilized. In the initial step, the occurrence of breast cancer emerged as a significant predictor, explaining 53% of the variance in anxiety (P<0.001). The second step introduced lifestyle factors, including sleep efficacy and PA level, with sleep efficacy proving to be a significant predictor. This extended model accounted for 57% of the variance in anxiety (P<0.001). In the third step, clinical outcomes (estrogen receptor expression, progesterone receptor expression, and HER2-positive status) were examined. Only sleep efficacy emerged as a significant predictor, explaining 59% of the variance in anxiety (P<0.001). The fourth step added age to the regression model, but no significant predictors were found. This final model accounts for 59% of the anxiety variance (P<0.001) (Table 5).
Discussion
Diagnostic difficulties combined with the high risk of poor mental state require effective methods for detecting and treating mental disorders in cancer patients. Preparing patients for therapy is crucial, as cancer therapies can be devastating. Oncological prehabilitation has become a topic of interest since it aims to increase motivation for PA and fitness. However, there are still no specific recommendations on how such prehabilitation should occur and on which aspects it should focus.
Our results provide a broad look at the characteristics of breast cancer patients. The average age of patients in the cancer group was in line with the prevailing literature, which confirms that the number of breast cancer cases in younger age groups is significantly increasing [35]. In addition, our descriptive statistics show the low epidemiological predictability of breast cancer.
The study included patients with varying financial situations, living standards, education levels, age, and BMI, which indicates that patients in different clinical conditions and stages of treatment may need psychotherapy. However, participants in the DG had a lower overall daily activity level according to the IPAQ scale. Unfortunately, it is unclear whether the lower activity levels are due to the diagnosis or are a cause of the disease. Based on current knowledge, it can be assumed that a lack of activity in these patients is an indirect cause and consequence of cancer. However, mental state, general health, and QOL varied substantially among individuals.
The need to supplement the prehabilitation process with psychotherapeutic elements was demonstrated in our previous research, which showed that PA is either a cause or result of reduced mental health [36]. The current findings could be meaningful in future research in this population. Indeed, improving PA parameters could be crucial for oncological prehabilitation and treatment.
The results of the current study clearly show that cancer patients struggle with anxiety and depression symptoms. In addition, their QOS is poor and PA is insufficient. Sleep and physical activity play a vital role in human health and healing. However, the relationships between the individual parameters have not yet been precisely described. According to Wu et al [37], sleep disturbances were most frequent, which is in line with our findings. Sleep disturbances significantly increased the risk of survivors’ fatigue and/or depressive mood after cancer treatment completion.
The results of a study by Civilotti et al [38] are also consistent with our reports. Of over 400 breast cancer patients from a single Italian medical center examined immediately after diagnosis, 52.1% had symptoms of anxiety and almost 1/3 had symptoms of depression, which shows the need to improve the standards of care in terms of psychological support starting at diagnosis. That study’s design slightly differed from our study protocol due to lack of a comparison group, but this does not change the fact that psychophysical well-being disorders are a common problem in Poland and worldwide.
Yang et al [39] found additional associations between the mental state and QOL of oncological patients. In a group of 300 patients, the authors examined the relationship between mental well-being and fear of relapse. Interestingly, they found that anxiety, depression, life stress, family cancer history, and pessimism predicted higher fear of cancer recurrence. These findings indicate that worse mental well-being during treatment or at diagnosis leads to significantly worse well-being and QOL, even years after treatment ends. This study confirms that patients need additional care focused on improving their QOL and overall mental well-being, even at the beginning of the disease.
Our regression analysis results show that mental health is a complex mechanism, and factors such as breast cancer occurrence, sleep efficacy, PA level, hormone levels, and physiological parameters can affect the regression models. Interestingly, participant age was not associated with mental health. Although the regression models explain certain relationships with great power and significance, the results also show that some factors may have an impact on women’s well-being that were not analyzed in our study. This again highlights the importance and complexity of the mental health problem of cancer patients.
According to our hypotheses, breast cancer patients present with symptoms of anxiety and depression, as well as sleep and mood disorders. The scale of this problem is clearly seen by comparison with healthy women.
Our study has several potential limitations. Subjectively assessed PA may not be a reliable indicator. However, the differences in this category are also clear to see, even if measured subjectively. Therefore, it would be worthwhile to use measurement tools that allow for an objective assessment of patients’ energy expenditure and activity and compare such results with patients’ health. Our study also lacked long-term assessment after initiation and completion of treatment. Finally, the non-random selection of breast cancer patients from a specific oncology center might introduce bias and restrict the generalizability of findings. However, we felt that the impact was not significant because patients were only diagnosed and were not subjected to extensive and lengthy medical procedures at a given facility.
Despite some limitations, this study presents a reliable image of the mental state and QOL of patients with breast cancer. Future studies should have a larger sample size, include more reference groups (chemotherapy, radiotherapy), and extend the diagnostics with more reliable and precise measurement tools. However, our results provide a foundation for the search for alternative, comprehensive, and, holistic therapeutic tools that have potential in oncological prehabilitation, prevention, and treatment. We believe that searching for engaging, effective ways to improve QOL, mental health, and PA is justified. The results confirm that anxiety, depression, QOS, and PA levels pose a serious threat to the health of patients diagnosed with breast cancer. Moreover, according to the regression analysis results, it seems reasonable to search for other predictors of mental health and QOL, not only in the selected direction. The results may also suggest ways to combat these issues, symptoms, disorders, and problems.
Conclusions
Anxiety, depression, poor QOS, and insufficient PA are common factors in patients with breast cancer. The mental state and well-being of healthy women seems to clearly differ from breast cancer patients. Breast cancer, QOS, level of PA, and clinical status potentially are important factors influencing the participants’ psychological symptoms. These findings confirm all the stated hypotheses. Further research is needed to explore the issue more extensively and determine whether any of the sociodemographic variables impact the measured parameters.
References
1. Veronesi G, Baldwin D, Henschke C, Recommendations for implementing lung cancer screening with low-dose computed tomography in Europe: Cancers, 2020; 12; 1672
2. Mattiuzzi C, Lippi G, Current cancer epidemiology: J Epidemiol Glob Health, 2019; 9(4); 217-22
3. Anders C, Johnson R, Litton J, Breast cancer before age 40 years: Semin Oncol, 2009; 36; 237-49
4. Nakatani Y, Iwamitsu Y, Kuranami MEmotional suppression and psychological responses to a diagnosis of breast cancer: Shinrigaku Kenkyu, 2012; 83(2); 126-34 [in Japanese]
5. Wang HH, Chung UL, Healthy lifestyle changes during the period before and after cancer diagnosis among breast cancer survivors: Asian Pac J Cancer Prev, 2012; 13(9); 4769-72
6. Mehnert A, Koch U, Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: A prospective study: Psychooncology, 2007; 16(3); 181-88
7. Loeffler S, Poehlmann K, Hornemann B, Finding meaning in suffering? – Meaning making and psychological adjustment over the course of a breast cancer disease: Eur J Cancer Care (Engl), 2018; 27(3); e12841
8. Little M, Sayers EJ, While there’s life… hope and the experience of cancer: Soc Sci Med, 2004; 59(6); 1329-37
9. Khan F, Amatya B, Pallant JF, Rajapaksa I, Factors associated with long-term functional outcomes and psychological sequelae in women after breast cancer: Breast, 2012; 21(3); 314-20
10. Mehnert A, Hartung TJ, Friedrich M, One in two cancer patients is significantly distressed: Prevalence and indicators of distress: Psychooncology, 2018; 27(1); 75-82
11. Krzyszczyk P, Acevedo A, Davidoff E, The growing role of precision and personalized medicine for cancer treatment: Technology (Singap World Sci), 2018; 6(3–4); 79-100
12. Bishayee A, Block K, A broad-spectrum integrative design for cancer prevention and therapy: The challenge ahead: Semin Cancer Biol, 2015; 35(Suppl); S1-S4
13. Poort H, Jacobs J, Pirl W, Fatigue in patients on oral targeted or chemotherapy for cancer and associations with anxiety, depression, and quality of life: Palliat Support Care, 2020; 18(2); 141-47
14. Baumann F, Bloch W, Weissen A, Physical activity in breast cancer patients during medical treatment and in the aftercare – a review: Breast Care (Basel), 2013; 8(5); 330-34
15. Furmaniak A, Menig M, Markes M, Exercise for women receiving adjuvant therapy for breast cancer: Cochrane Database Syst Rev, 2016; 9(9); CD005001
16. Poort H, van der Graaf W, Tielen R, Prevalence, impact, and correlates of severe fatigue in patients with gastrointestinal stromal tumors: J Pain Symptom Manage, 2016; 52(2); 265-71
17. Bray F, Ferlay J, Soerjomataram I, Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries: Cancer J Clin, 2018; 68; 394-424
18. Torrisi M, De Cola M, Buda A, Self-efficacy, poststroke depression, and rehabilitation outcomes: Is there a correlation?: J Stroke Cerebrovasc Dis, 2018; 27; 3208-11
19. Epstein N, Multidisciplinary in-hospital teams improve patient outcomes: A review: Surg Neurol Int, 2014; 5; S295-S303
20. Loef M, Paepke D, Walach H, Quality of life in breast cancer patients treated with mistletoe extracts: A systematic review and meta-analysis: Integr Cancer Ther, 2023; 22; 15347354231198074
21. Saevarsdottir S, Gudmundsdottir S, Mobile apps and quality of life in patients with breast cancer and survivors: Systematic literature review: J Med Internet Res, 2023; 25; e42852
22. Javan Biparva A, Raoofi S, Rafiei S, Global depression in breast cancer patients: Systematic review and meta-analysis: PLoS One, 2023; 18(7); e0287372
23. Krok D, Telka E, Moroń M, Marital satisfaction, partner communication, and illness acceptance among couples coping with breast cancer: A dyadic approach: Psychooncology, 2023; 32(8); 1240-47
24. Sun M, Liu C, Lu Y, Effects of physical activity on quality of life, anxiety and depression in breast cancer survivors: A systematic review and meta-analysis: Asian Nurs Res (Korean Soc Nurs Sci), 2023; 17(5); 276-85
25. Diao X, Ling Y, Zeng Y, Physical activity and cancer risk: A dose-response analysis for the Global Burden of Disease Study 2019: Cancer Commun (Lond), 2023; 43(11); 1229-43
26. Barnes L, Harp D, Jung W, Reliability generalization of scores on the Spielberger State-Trait Anxiety Inventory: Educational and Psychological Measurement, 2002; 62(4); 603-18
27. Beck A, Ward C, Mendelson M, Mock J, Erbaugh J, An inventory for measuring depression: Arch Gen Psychiatry, 1961; 4; 561-71
28. Hallal P, Victora C, Reliability and validity of the International Physical Activity Questionnaire (IPAQ): Med Sci Sports Exerc, 2004; 36; 556
29. Mollayeva T, Thurairajah P, Burton K, The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis: Sleep Med Rev, 2016; 25; 52-73
30. Fortin J, Leblanc M, Elgbeili G, The mental health impacts of receiving a breast cancer diagnosis: A meta-analysis: Br J Cancer, 2021; 125(11); 1582-92
31. Gustafson LW, Gabel P, Hammer A, Validity and reliability of State-Trait Anxiety Inventory in Danish women aged 45 years and older with abnormal cervical screening results: BMC Med Res Methodol, 2020; 20(1); 89
32. García-Batista ZE, Guerra-Peña K, Cano-Vindel A, Validity and reliability of the Beck Depression Inventory (BDI–II) in general and hospital population of Dominican Republic: PLoS One, 2018; 13(6); e0199750
33. Hagströmer M, Oja P, Sjöström M, The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity: Public Health Nutr, 2006; 9(6); 755-62
34. Casement MD, Harrington KM, Miller MW, Resick PA, Associations between Pittsburgh Sleep Quality Index factors and health outcomes in women with posttraumatic stress disorder: Sleep Med, 2012; 13(6); 752-58
35. Siegel R, Miller K, Fuchs H, Jemal A, Cancer statistics, 2021: Cancer J Clin, 2021; 71(1); 7-33
36. Czech O, Siewierska K, Krzywińska A, Virtual therapy complementary prehabilitation of women diagnosed with breast cancer – a pilot study: Int J Environ Res Public Health, 2022; 20(1); 722
37. Wu H, Gao F, Given C, Living as a survivor: Sleep disturbance, fatigue, depressive mood, and cognitive dysfunction after breast cancer treatment: Cancer Nurs, 2023 [Online ahead of print]
38. Civilotti C, Acquadro Maran D, Santagata F, The use of the Distress Thermometer and the Hospital Anxiety and Depression Scale for screening of anxiety and depression in Italian women newly diagnosed with breast cancer: Support Care Cancer, 2020; 28(10); 4997-5004
39. Yang Y, Qi H, Li W, Predictors and trajectories of fear of cancer recurrence in Chinese breast cancer patients: J Psychosom Res, 2023; 166; 111177
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952