02 May 2022: Clinical Research
Effect of Intracameral Carbachol and Epinephrine Use on Choroidal Thickness After Uncomplicated Phacoemulsification
Hasan Burhanettin Kaptı1ABEF*, Serkan Özen2CD, Mustafa Gök3EFDOI: 10.12659/MSM.935315
Med Sci Monit 2022; 28:e935315
Abstract
BACKGROUND: Safety concerns about drugs used intracamerally during cataract surgery have been the subject of many studies. In this study, the effect of using intracameral carbachol and epinephrine on choroidal thickness was evaluated.
MATERIAL AND METHODS: This prospective interventional study included 81 eyes of 81 patients undergoing cataract surgery. During cataract surgery, intracameral carbachol was administered to 27 eyes, intracameral epinephrine was administered to 20 eyes, and 34 eyes were the control group. Macular choroidal thickness measurement was performed before, 1 day, and 1 week after phacoemulsification surgery in all patients using optical coherence tomography.
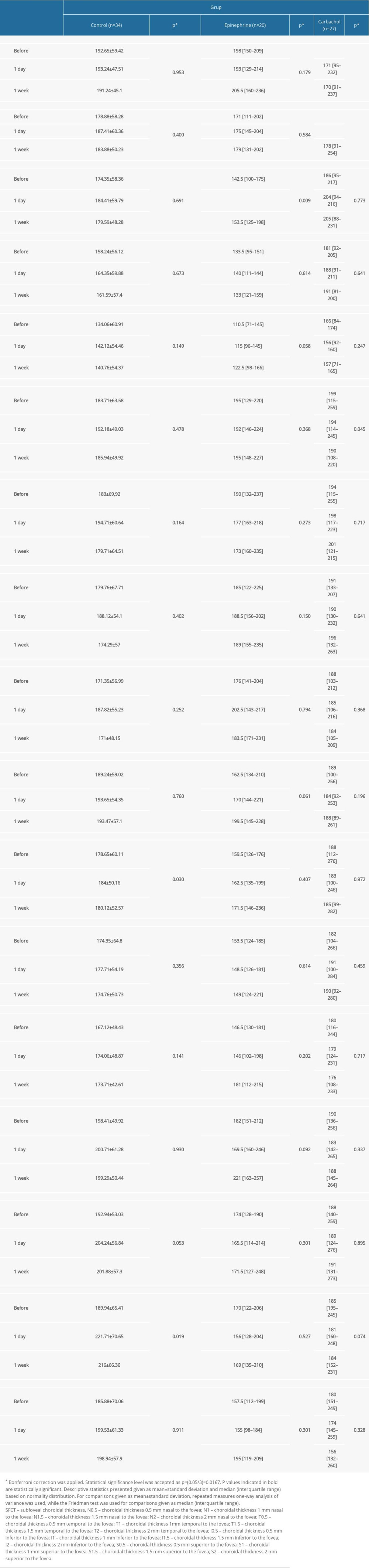
RESULTS: Subfoveal choroidal thickness was significantly reduced at day 1 and week 1 in the group receiving intraoperative carbachol compared with preoperative measurement (P=0.016). In addition, choroidal thickness in the 500 µm nasal fovea was significantly reduced in the carbachol group at 1st week compared to the preoperative measurement (P=0.008). There was no significant difference in postoperative subfoveal thickness in the intraoperative epinephrine group and control group (P=0.179 and P=0.953, respectively). Choroidal thickness at 1000 µm nasal fovea was significantly higher in the epinephrine group at postoperative 1st day than preoperative and postoperative 1st week values (P=0.009).
CONCLUSIONS: The use of intracameral epinephrine caused an increase in choroidal thickness 1000 µm nasal of the fovea, while intracameral carbachol caused thinning in the subfoveal and 500 µm nasal quadrant. Intracameral drug administration during cataract surgery may be associated with posterior segment complications.
Keywords: carbachol, Choroid, Epinephrine, Phacoemulsification, Tomography, Optical Coherence, Cataract, Humans, Prospective Studies
Background
Carbachol is a parasympathomimetic drug that binds to and activates acetylcholine receptors. By binding to muscarinic acetylcholine receptors in the eye, it performs many functions such as regulation of pupil size, regulation of intraocular pressure (IOP), cell-to-cell signal transmission, and modulation of vessel diameter [1]. Carbachol is used intracamerally during ophthalmic surgery for postoperative IOP control by inducing miosis and preventing iris entrapment at incision sites. Epinephrine, in contrast, is a substance that causes mydriasis with a dual effect by affecting the α-receptor, causing the dilator muscles to contract, and by affecting the β-receptor, causing the sphincter to relax. Epinephrine is used intracamerally to cause mydriasis during cataract surgery and to reduce the risk of iris damage in patients with intraoperative floppy iris syndrome [2].
Safety concerns regarding intracamerally administered drugs have been the subject of many studies. Studies have focused specifically on retinal and endothelial toxicity. While intracameral carbachol does not cause corneal endothelial cell damage, it has been shown to reduce macular thickness and volume in the early postoperative period [3]. In addition, animal studies have shown that carbachol causes dilatation of retinal vessels [4]. It has been shown that the use of intracameral epinephrine poses a risk for macular edema and endothelial toxicity [5]. Because the choroid is a vascular tissue closely associated with the retina, providing nutrition and oxygenation of the retina, events affecting the retina are likely to affect the choroid as well. Nickla et al showed in their animal study that intravitreal carbachol causes thinning of the choroid by affecting muscarinic receptors [6]. Thus, we can predict that a similar effect can be observed after intracamerally administered carbachol.
Studies have shown that phacoemulsification surgery affects choroidal thickness [7–11]. However, to the best of our knowledge, there is no study evaluating the effects of intracamerally administered carbachol and epinephrine on choroidal thickness.
The aim of this study was to evaluate the effect of intracamerally administered epinephrine and carbachol on choroidal thickness in the early period during uncomplicated phacoemulsification surgery.
Material and Methods
STUDY POPULATION:
Patients were assigned to 1 of the 3 groups by simple randomization method using computer-generated random numbers. Groups were changed from day to day in a predetermined order until the number of patients in the smallest group reached 20. The patients were unaware of which group they were assigned to. This study consisted of 3 groups: the epinephrine group, the carbachol group, and the control group. Intracameral carbachol and epinephrine was not used for complication management. In the epinephrine group, 0.2 mL of epinephrine (1: 5000 solution) was used immediately after making the clear corneal incision. In the carbachol group, a 0.5-ml dose of 0.01% carbachol solution (Miostat®, Alcon Laboratories, Inc., Fort Worth, TX) was given intracamerally immediately after viscoelastic matter removal following IOL implantation. The control group was given neither epinephrine nor carbachol. Patients with systemic diseases such as hypertension and diabetes, ocular problems such as uveitis, glaucoma, amblyopia, maculopathy, retinal dystrophy, any previous ocular surgery, eye trauma, and eyes with congenital cataracts were excluded from the study. In addition, eyes with media opacity and mature cataracts that prevented the OCT evaluation of the macula, eyes with intraoperative complications (posterior capsule rupture, prolonged phaco time, or iris trauma), and postoperative complications (fibrin reaction or posterior capsule opacity) were not included in the study.
EYE EXAMINATIONS:
Best corrected visual acuity using a Snellen chart, axial length measurement, IOP measurement using a non-contact tonometer, anterior and posterior segment examinations using a slit lamp, and macular choroidal thickness (MCT) measurement using OCT were performed in all patients before, 1 day after, and 1 week after phacoemulsification surgery.
MCT measurement was performed by an experienced technician preoperatively, on postoperative day 1, and in postoperative week 1 after pupil dilation with 1% tropicamide and 2.5% phenylephrine using a Cirrus HD 500 spectral OCT platform (Carl Zeiss Meditec, Dublin, CA, USA). All MCT measurements were made at the same daily interval (10–11 a.m.) to avoid diurnal variation. Subfoveal, nasal, temporal, lower choroidal thickness, and upper choroidal thickness were measured manually by 2 blinded observers with 0.5-mm intervals in vertical and horizontal sections having a length of 4 mm. The distance between the outer hyper-reflective border of the retinal pigment epithelium and the inner scleral surface was considered. Average data obtained by 2 observers were used in statistical analysis.
SURGICAL TECHNIQUE:
Mydriasis was induced using combined 2.5% phenylephrine and 1.0% tropicamide topical drops before surgery. All surgeries were performed by the same surgeon (HBK) using a similar technique, under topical anesthesia (0.05% proparacaine HCL), and with a 2.8-mm temporal clear corneal incision. After making the incision, 0.2 mL of preservative-free epinephrine (1: 5000) was injected into the epinephrine group only. A combination of 1.6% sodium hyaluronate and 4% chondroitin sulfate (ophthalmic viscosurgical device, Discovisc, Alcon Laboratories, Inc.) was used during capsulorrhexis in all 3 groups, and Alcon Infiniti System (Alcon Laboratories, Inc.) was used for phacoemulsification. A continuous curvilinear capsulorrhexis of 4.5–5.5 mm was created. After complete hydrodissection, the nucleus was removed using the stop and chop technique. Phacoemulsification time (range: 30–60 s) was similar in all patients, while the phacoemulsification strength was set to 35–40% for all operations. The cortex was aspirated in irrigation/aspiration mode. Before implanting a one-piece foldable hydrophobic acrylic IOL into the capsular bag, 1% sodium hyaluronate (ophthalmic viscosurgical device, Healon) was injected into the capsular bag. After removal of the viscoelastic material, only the carbachol group was given 0.5 ml of 0.01% carbachol solution intracamerally. Hydration with balanced salt solution was used to close the corneal incisions. Topical moxifloxacin, nepafenac, and prednisolone acetate eye drops were given to all patients 6 times a day for the first week. Prednisolone acetate was then reduced and discontinued 4 weeks after the operation.
STATISTICAL ANALYSIS:
Sample size was calculated before including the first patient. With a=0.05 and a power of 90%, 20 patients were calculated as the minimum requirement for each group. However, more patients were included in the study to increase reliability and ensure sufficient working power. In summarizing data from the study, descriptive statistics were presented as mean±standard deviation or median [interquartile range] for continuous variables, depending on the distribution. Categorical variables were summarized as numbers and percentages. The normality of numerical variables was checked using the Kolmogorov-Smirnov test. Preoperative, day 1, and week 1 measurements in each group were evaluated separately and repeated measures one-way analysis of variance was used for parameters with normal distribution, whereas the Friedman test was used for parameters that did not show normal distribution. Multiple comparisons were evaluated using the Durbin-Conover test. One-way analysis of variance was used for independent groups to determine whether there was a statistically significant difference between the mean age and axial measurements of the groups. The Fisher-Freeman-Halton test was used for comparison of sex distributions according to groups.
The ‘R Commander’ and ‘RcmdrPlugin.KMggplot2’ packages in the R programming language (v3.6.0) were used to create the charts.
Statistical analyses were performed with the Jamoviproject (2019) (Jamovi (Version1.0.1) Computer Software (Retrieved from
Results
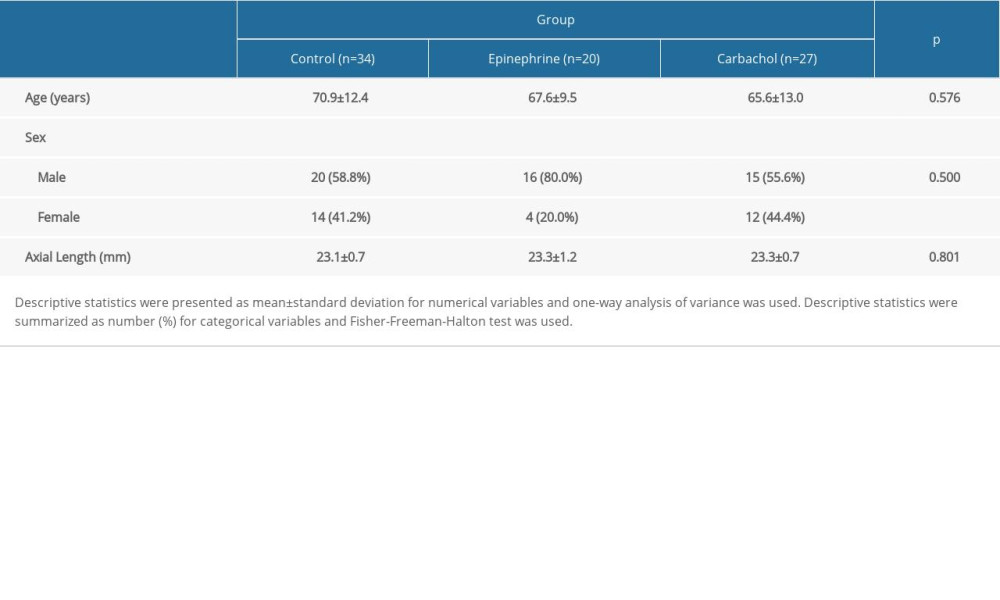
There was no significant difference between the groups in terms of age, sex, and preoperative axial length (
Subfoveal choroidal thickness at day 1 and week 1 was significantly reduced in the group receiving intraoperative carbachol compared with the preoperative subfoveal choroidal thickness (
Postoperative fibrin reaction, endophthalmitis, bullous keratopathy, cystoid macular edema, or severe ocular hypertension did not develop in any eye.
Discussion
Phacoemulsification is the most commonly performed surgical procedure in ophthalmology. Cataract surgery is known to cause some adverse effects on the retina, such as progression in diabetic retinopathy, pseudophakic cystoid macular edema, and progression in age-related macular degeneration. Studies have shown that phacoemulsification surgery increases choroidal thickness. It is proposed that the increase in inflammation caused by the release of proinflammatory molecules after phacoemulsification surgery increases the choroidal thickness [8,9]. In the present study, non-significant increases in choroidal thickness were observed in all quadrants on postoperative day 1 in the control group. At postoperative week 1, some quadrants showed an increase in thickness compared with the preoperative and postoperative day 1 values, whereas a decreasing trend was observed in the other quadrants compared with the postoperative day 1 values. These results obtained from the control group are consistent with the literature. In our study, while no significant changes were observed in choroidal thickness in the control group, significant changes were observed in choroidal thickness in some quadrants in the carbachol and epinephrine group. This shows us that complicated cataract surgeries using carbachol and epinephrine can cause more significant effects on the choroid than standard cataract surgery. This effect may be more critical, particularly in eyes with diabetic retinopathy, age-related macular degeneration.
Studies evaluating the effects of intracameral carbachol have generally focused on its effects on intraocular pressure [12–14]. It was shown in a study that it had no effect on posterior capsule opacification [15]. There are few studies evaluating the effects of intracamerally administered carbachol on the retina during cataract surgery. In a study evaluating the effect of carbachol given during uncomplicated cataract surgery on central macular thickness, total macular volume, and retinal vessel diameter, it was found that it reduced macular thickness and volume in the early postoperative period, but had no effect on retinal vessel diameter [3]. Demir et al, on the other hand, found that intracameral carbachol had no effect on the foveal thickness at the postoperative 4th week [16]. In a few studies evaluating the safety of intracameral epinephrine use, its effects on intraocular pressure and cardiovascular parameters were evaluated and no significant effect was observed [17–19]. Bamdad et al evaluated the effect of different concentrations of intracameral epinephrine on macular thickness and found that epinephrine at high concentration caused a significant increase in macular thickness compared to the control group [5].
In animal studies, intravitreally administered carbachol was shown to cause a significant reduction in choroidal thickness in in vivo and in vitro measurements within 3 h after injection. While the effect of carbachol on the choroid in the first 24 h was dose-dependent, no difference was observed between the experimental and control groups 48 h after the injection [6]. Pekel et al found that 0.01% carbachol administered intracamerally during phacoemulsification surgery reduced the total macular volume in the early period. The effect of carbachol on the macula in postoperative week 1 and postoperative month 1 was similar to that in the control group [3]. Results obtained in the early period in the present study are similar to those in these studies [3,6]. These results suggest that the effect of intracamerally administered carbachol is not long-lasting.
The effect of carbachol on the choroid may occur through various mechanisms. First, postoperative IOP decrease due to carbachol may increase ocular perfusion and increase choroidal thickness [12]. Second, the use of intracameral carbachol may increase choroidal thickness by increasing inflammation [20]. Third, it may be via muscarinic acetylcholine receptors. Muscarinic acetylcholine receptors consist of 5 subtypes, namely M1, M2, M3, M4, and M5, and all of them are expressed in the retina [21]. The subtypes of muscarinic receptors have also been shown in the choroid in animal studies [20]. Choroidal thickness can be affected by these receptors on the choroid, which may also be present in humans. In the present study, when the control group and the carbachol group were compared, significant thinning was found only in the subfoveal and 500 μm nasal quadrants in the carbachol group. No significant change was observed in the other quadrants. According to the results of our study, it can be considered that carbachol reduces choroidal thickness with its direct effect on the choroid through muscarinic receptors and increases choroidal thickness indirectly by changing IOP and inflammation parameters. As a result, this antagonist effect reduces choroidal thickness.
We found a significant reduction in the subfoveal and 500 μm nasal quadrants in the carbachol group, and a similar reduction in choroidal thickness was observed in most other quadrants, although not significantly. A significant increase was observed only in the 1000 μm nasal quadrant in the epinephrine group, and similarly, the choroidal thickness increased in the other quadrants, although it was not significant. Inconsistent results were seen in some choroidal quadrants, although they were not statistically significant in either group. We cannot exclude that the different results between groups and inconsistent results in different quadrants within the group may be due to artifacts in retinal imaging. Cohen et al suggested that lenticular opacities may lead to different results by causing artifacts in retinal imaging [22]. In addition, in the study evaluating the effect of intracameral carbachol on retinal vessel diameter and total macular volume, the authors emphasized that the difference between the control group and the carbachol group may be due to optical factors, since the pupil of the carbachol group was smaller on the 1st postoperative day compared to the control group [3]. However, the homogeneous nature of the patients included in our study, the exclusion of mature cataracts that may affect the results of our study, the blinding of the patients and the investigator who evaluated the results are the factors that make our study strong, and these results may provide important contributions to future studies that will evaluate the effects of intracameral carbachol and epinephrine on the posterior segment. Stronger evidence can be obtained with a larger sample size and longer follow-up.
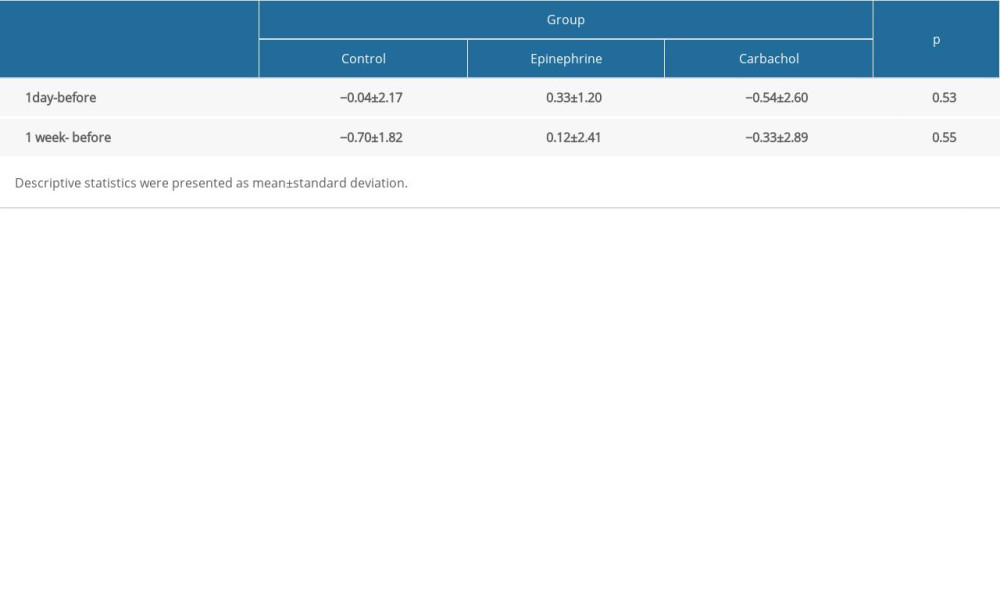
Studies have shown that carbachol given intracamerally during cataract surgery provides a significant decrease in IOP in the early postoperative period and prevents IOP increase [12,18]. In our study, there was a decrease in IOP values on the postoperative 1st day and 1st week in the carbachol group compared to the preoperative measurement, but this difference was not statistically significant. On the other hand, in an animal study evaluating the postoperative results of intracameral epinephrine, no statistically significant difference was observed between the epinephrine group and the saline group [15]. In our study, similar to that study, no statistically significant difference was observed between the epinephrine group and the control group. The results of our study do not indicate the possible effect of IOP change on choroidal thickness.
The ophthalmic use of epinephrine, a sympathomimetic drug widely used in intraocular surgery, reduces blood flow to the ciliary body and choroid and lowers intraocular pressure [24]. In a study on monkeys, Cheong et al found that systemic use of adrenaline caused a statistically significant increase in subfoveal choroidal thickness [25]. Another study showed that the use of topical mydriatics caused a significant increase in subfoveal choroidal thickness compared with that in the control group [26]. In a study evaluating the effect of intracamerally used epinephrine at different concentrations on macular thickness, it was shown that 1: 10 000 epinephrine caused a significant increase in macular thickness compared with the control group and 1: 100 000 epinephrine group [5]. In the present study, epinephrine was used at a concentration of 1: 5000, and the choroidal thickness was significantly higher in the 1000 μm nasal fovea on postoperative day 1 compared with the preoperative and postoperative week 1 values. In our study, consistent with the literature, a significant increase in choroidal thickness was observed in the 1000 mm nasal fovea after intracameral epinephrine administration on the postoperative 1st day compared to the preoperative and postoperative 1st week.
There are certain limitations of this study. The first limitation is that inflammation parameters were not evaluated. It has been reported that inflammatory disorders due to focal and systemic diseases may affect choroidal thickness. It has also been shown that cataract surgery causes an inflammatory response and affects choroidal thickness [7]. Previous studies also show that intraocular carbachol causes postoperative inflammation [20]. These results highlight the importance of evaluating inflammation parameters. The second limitation is that our postoperative choroidal thickness measurements were limited to day 1 and week 1. We do not know how the choroidal thickness changes in the long term. The third limitation is the sample size differences between groups, which may have affected the significance of the results.
Conclusions
Intraoperative use of carbachol caused a significant reduction in choroidal thickness in the subfoveal and 500 μm nasal quadrants. Intraoperative use of adrenaline caused an increase in choroidal thickness in the nasal quadrant 1000 μm away from the fovea centralis. Drugs such as carbachol and epinephrine administered intracamerally during cataract surgery may increase the severity of retinal disorders such as age-related macular degeneration and diabetic retinopathy by changing posterior segment structures such as the retina and choroid, and it may also be associated with an increased risk of post-surgical complications such as pseudophakic cystoid macular edema. Therefore, in retinal diseases such as age-related macular degeneration and diabetic retinopathy, especially during complicated cataract surgery, using drugs such as carbachol and epinephrine in appropriate doses and not using them unless necessary can minimize the possible adverse effects of these drugs. Studies in which the effects of intracameral drug use during cataract surgery on eyes with retinal disorders such as DR and AMD are observed and the postoperative risk increase is evaluated can provide important information about the safe use of these drugs. Prospective studies with larger patient groups and long-term follow-up measurements are required to evaluate the effect of intraoperative use of carbachol and adrenaline on choroidal thickness.
References
1. Ruan Y, Patzak A, Pfeiffer N, Muscarinic acetylcholine receptors in the retina-therapeutic implications: Int J Mol Sci, 2021; 22; 4989
2. Yu AY, Guo H, Wang QM, Pupil dilation with intracameral epinephrine hydrochloride during phacoemulsification and intraocular lens implantation: J Ophthalmol, 2016; 2016; 4917659
3. Pekel G, Yagci R, Acer S, Effect of intracameral carbachol in phacoemulsification surgery on macular morphology and retinal vessel caliber: Cutan Ocul Toxicol, 2015; 34; 42-45
4. Gericke A, Sniatecki JJ, Goloborodko E, Identification of the muscarinic acetylcholine receptor subtype mediating cholinergic vasodilation in murine retinal arterioles: Invest Ophthalmol Vis Sci, 2011; 52; 7479-84
5. Bamdad S, Khalili MR, Rahimi R, Comparison of the effects of 1/10,000 and 1/100,000 concentrations of intracameral epinephrine on corneal endothelium and macular thickness after uncomplicated phacoemulsification: Eye (Lond), 2020; 34; 2300-306
6. Nickla DL, Zhu X, Wallman J, Effects of muscarinic agents on chick choroids in intact eyes and eyecups: Evidence for a muscarinic mechanism in choroidal thinning: Ophthalmic Physiol Opt, 2013; 33; 245-56
7. Zeng S, Liang C, He Y, Changes of subfoveal choroidal thickness after cataract surgery: A meta-analysis: J Ophthalmol, 2018; 2018; 2501325
8. Yılmaz T, Karci AA, Yilmaz İ, Long-term changes in subfoveal choroidal thickness after cataract surgery: Med Sci Monit, 2016; 22; 1566-70
9. Aslan Bayhan S, Bayhan HA, Muhafiz E, Evaluation of choroidal thickness changes after phacoemulsification surgery: Clin Ophthalmo, 2016; 10; 961-67
10. Gudauskiene G, Matuleviciute I, Mockute R, Changes in subfoveal choroidal thickness after uncomplicated cataract surgery: Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 2019; 163; 179-83
11. Ibrahim AM, Elgouhary SM, Nassar MK, Changes in choroidal thickness after cataract surgery: Semin Ophthalmol, 2018; 33; 664-70
12. Cekiç O, Batman C, Effect of intracameral carbachol on intraocular pressure following clear corneal phacoemulsification: Eye (Lond), 1999; 13; 209-11
13. Wedrich A, Menapace R, Effect of carbachol on intraocular pressure in small-incision cataract surgery: Doc Ophthalmol, 1992; 80; 301-7
14. Ruiz RS, Rhem MN, Prager TC, Effects of carbachol and acetylcholine on intraocular pressure after cataract extraction: Am J Ophthalmol, 1989; 107; 7-10
15. Phillips B, Crandall AS, Mamalis N, Olson RJ, Intraoperative miotics and posterior capsular opacification following phacoemulsification with intraocular lens insertion: Ophthalmic Surg Lasers, 1997; 28; 911-14
16. Demir M, Oba E, Dirim B, Effect of intracameral carbachol given during cataract surgery on macular thickness: Int Ophthalmol, 2012; 32; 413-16
17. Amorim TM, Dower NMB, Stocco MB, Effects of intracameral injection of epinephrine and 2% lidocaine on pupil diameter, intraocular pressure, and cardiovascular parameters in healthy cats: Vet Ophthalmol, 2019; 22; 276-83
18. Alabdulwahhab KM, Efficacy and effect of intracameral adrenaline infusion on pulse rate and blood pressure during phacoemulsification in patients with dark irides: Eur Rev Med Pharmacol Sci, 2021; 25; 4773-78
19. Osinchuk SC, Salpeter EM, Lavallee G, Effect of intracameral epinephrine on heart rate, post-operative ocular hypertension, and long-term outcome following canine phacoemulsification: Vet Ophthalmol, 2020; 23; 872-78
20. Roberts CW, Intraocular miotics and postoperative inflammation: J Cataract Refract Surg, 1993; 19; 731-34
21. Mitchelson F, Muscarinic receptor agonists and antagonists: Effects on ocular function: Handb Exp Pharmacol, 2012; 208; 263-98
22. Cohen KL, Patel SB, Ray N, Retinal thickness measurement after phacoemulsification: J Cataract Refract Surg, 2004; 30; 1501-6
23. Stuhr CM, Miller PE, Murphy CJ, Effect of intracameral administration of carbachol on the postoperative increase in intraocular pressure in dogs undergoing cataract extraction: J Am Vet Med Assoc, 1998; 12; 1885-88
24. Osinchuk SC, Salpeter EM, Lavallee G, Effect of intracameral epinephrine on heart rate, post-operative ocular hypertension, and long-term outcome following canine phacoemulsification: Vet Ophthalmol, 2020; 23; 872-78
25. Cheong KX, Barathi VA, Teo KYC, Choroidal and retinal changes after systemic adrenaline and photodynamic therapy in non-human primates: Invest Ophthalmol Vis Sci, 2021; 62; 25
26. Öner V, Bulut A, Öter K, The effect of topical anti-muscarinic agents on subfoveal choroidal thickness in healthy adults: Eye (Lond), 2016; 30; 925-28
In Press
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952